PAHO/WHO | Pan American Health Organization
PAHO and CAF to work together to strengthen health systems in Latin America and the Caribbean
PAHO and CAF to work together to strengthen health systems in Latin America and the Caribbean
Cristina Mitchell
19 Sep 2023
PAHO and CAF to work together to strengthen health systems in Latin America and the Caribbean
Cristina Mitchell
19 Sep 2023
1 year 10 months ago
PAHO/WHO | Pan American Health Organization
PAHO and PATH sign agreement to advance health equity in the Americas
PAHO and PATH sign agreement to advance health equity in the Americas
Cristina Mitchell
19 Sep 2023
PAHO and PATH sign agreement to advance health equity in the Americas
Cristina Mitchell
19 Sep 2023
1 year 10 months ago
Health Archives - Barbados Today
NCD Commission supports front-of-package warning labels
The Barbados National NCD Commission unreservedly supports the urgent call for the introduction of the Octagonal “high-in” front-of-package warning labels to be placed on pre-packaged food and beverage products. The octagonal warning label (OWL) is the best label for Barbados and the Caribbean.
Global and regional scientific evidence, conducted by researchers free from conflicts of interest, supports the OWL as the best option to empower consumers to correctly, quickly and easily identify foods high in sugars, sodium and fats. The OWL has consistently outperformed other front-of-package nutrition labels such as the magnifying glass, the traffic lights and the facts upfront. Research just released shows that the OWL has the potential to avert 16 per cent of the deaths caused by diet-related non-communicable diseases (NCDs).
The support of the Barbados National NCD Commission comes against a backdrop of an epidemic of obesity and NCDs across our region and in Barbados.
80% of deaths in Barbados are caused by NCDs and 76% of premature deaths are caused by this group of diseases.
31% of our children are overweight or obese.
66% of adults are overweight and 33% are obese.
1 in 5 adult Barbadians has diabetes.
We can no longer afford to ignore these dangerous trends affecting the health and well-being of the citizens of this country. We must become more conscious of ensuring the health and wellness of every one of us is taken seriously.
An unhealthy diet dominated by ultra-processed products high in sugars, sodium and fats is the single greatest risk factor for overweight, obesity and NCDs. Overconsumption of these foods drastically increases the risk of developing hypertension, obesity, type 2 diabetes, heart disease and some types of cancer.
Consumers make purchasing decisions in a matter of seconds, and it takes far too much time to understand the nutrition facts panel on the back of packaged products. Especially now, we need octagonal warning labels on the front of our food packages to easily identify food that has excess levels of key nutrients – especially for people who are living with NCDs such as diabetes, hypertension and cancer.
As the labels are now, it is very unlikely that most shoppers read food labels as they are often confusing and misleading. Having the octagonal “high-in” front-of-package labelling prominently displayed and easily readable will allow the consumer to make informed choices. This type of labelling is hard to ignore.
The health implications and the costs to fight NCDs and other diseases far outweigh the costs to manufacturers in implementing changes to their labels. We have over the years heard the cries from Ministries of Health across the region of the burgeoning costs of healthcare and the billions spent annually dealing with increasing cases of NCDs among our vulnerable population. The introduction of policies such as OWL can save the Government in excess of a billion Barbados dollars as predicted by the aforementioned study.
The octagonal warning label, recommended by PAHO/WHO and CARPHA, is a foundational and enabling policy which forms part of a comprehensive package of evidence-based policy actions aimed at creating healthy food environments in which healthy food is accessible, affordable, attractive, and widely available to all citizens regardless of socio-economic status. The OWL complements the recently introduced Barbados National School Nutrition Policy by providing the information needed to allow school administrators to readily identify foods which should be permitted in school settings.
Right now, CARICOM countries including Barbados, are voting on whether or not to approve a regional standard for the labelling of prepackaged foods which contains the octagonal warning label. Our Commission commends the Barbados Government as one of the governments in our region to vote yes for the Front-of-Package Warning Labels Octagonal System in 2021. As CARICOM continues to review this process, we want our collective voices to be heard and to resonate across the Caribbean in support of front-of-package warning labels.
Silence is no longer an option. Inaction cannot be the solution.
There is a clear and present danger to the health and well-being of our citizens from the onslaught of unhealthy foods and beverages.
Suleiman Bulbulia STE JP
Chairman
The post NCD Commission supports front-of-package warning labels appeared first on Barbados Today.
1 year 10 months ago
A Slider, Health, Health Care
Positive topline results show Botox Cosmetic may improve aesthetics of platysma prominence
Allergan Aesthetics, an AbbVie company, announced in a press release positive topline results from the second of three phase 3 studies evaluating Botox Cosmetic for the treatment of moderate to severe platysma prominence.The phase 3 trial, M21-310, found that Botox Cosmetic (onabotulinumtoxinA) demonstrated statistically significant improvement to platysma prominence, an aesthetically unappeali
ng condition that disrupts the neck, jawline and lower face of individuals due to a contraction of the platysma muscle, according to the press release.“Platysma prominence occurs as part of the
1 year 10 months ago
Medical News, Health News Latest, Medical News Today - Medical Dialogues |
'Overwhelming' bleeding reduction with abelacimab versus rivaroxaban in AF leads to early halting of trial
USA: Abelacimab, a novel factor XI/XIa inhibitor being studied in the AZALEA-TIMI 71 trial, was shown to lower a composite of major and clinically relevant nonmajor bleeding versus rivaroxaban in atrial fibrillation (AF) patients at a moderate-to-high-risk-of stroke. The results were announced by the drug's manufacturer Anthos Therapeutics.
Abelacimab is a novel, highly selective, fully human monoclonal antibody with dual inhibitory activity against factor XI and its active form, factor XIa.
The AZALEA-TIMI 71 trial stopped early due to an unprecedented bleeding benefit for adults with AF. The company noted that abelacimab is also the first and only factor XI inhibitor to demonstrate an unprecedented reduction in major bleeding compared with a DOAC (direct oral anticoagulant).
"The study was stopped by the data monitoring committee after it met its primary endpoint, a composite of major and clinically relevant nonmajor bleeding, in participants taking abelacimab versus patients taking rivaroxaban (Xarelto, Janssen/Bayer), a factor X inhibitor and a leading standard-of-care DOAC," Anthos stated in a press release.
“The AZALEA-TIMI 71 study is the largest and longest head-to-head study of a factor XI inhibitor to provide definitive evidence of a highly significant reduction in bleeding as compared to the standard-of-care anticoagulant,” Marc S. Sabatine, MD, MPH, the Lewis Dexter, MD, Distinguished Chair in Cardiovascular Medicine, Brigham and Women’s Hospital, professor at Harvard Medical School and chairman of the TIMI Study Group, said in the release.
“With a median of 21 months of follow-up, spanning more than 2,000 patient-years, AZALEA-TIMI 71 represents a landmark study confirming the promise of factor XI inhibition as causing substantially less bleeding than a current standard-of-care.”
The trial enrolled 1,287 patients from 95 centres in Asia, Europe, and North America and had a median of 21 months of follow-up before being stopped. Patients were randomized to receive either 20 mg oral daily rivaroxaban or 150 mg or 90 mg subcutaneous abelacimab every month.
According to Anthos Therapeutics, the full findings of the AZALEA-TIMI 71 will be presented at an upcoming scientific congress.
Just recently, the company announced that abelacimab had received a fast-track designation from the US FDA for the prevention of systemic embolism and stroke in AF patients. The fast-track designation is granted to therapies with the potential to fill the unmet needs of patients with serious medical conditions.
The investigational drug is a highly selective, fully human monoclonal antibody with dual inhibition against factor XI and factor XIa. It is not currently approved for any indication in any country.
Reference:
Verhamme P, et al. N Engl J Med. 2021;doi:10.1056/NEJMoa2105872.
1 year 10 months ago
Cardiology-CTVS,Medicine,Neurology and Neurosurgery,Cardiology & CTVS News,Medicine News,Neurology & Neurosurgery News,Top Medical News,Latest Medical News
Prostate cancer signs, symptoms and lifestyle changes that could reduce your risk
Prostate cancer is a disease found in men that develops in the prostate gland.
One in eight men will be diagnosed with prostate cancer in their lifetime, according to the American Cancer Society (ACS), with older men more likely to develop the disease.
Prostate cancer is a disease found in men that develops in the prostate gland.
One in eight men will be diagnosed with prostate cancer in their lifetime, according to the American Cancer Society (ACS), with older men more likely to develop the disease.
Prostate cancer is second only to skin cancer as the most common cancer diagnosed in men, according to the source.
OVARIAN CANCER SIGNS, SYMPTOMS, DIAGNOSIS AND TREATMENT OPTIONS
Symptoms of prostate cancer are typically very minimal, or not experienced at all.
Below is all you need to know about prostate cancer.
Any type of cancer starts when cells grow out of control in certain parts of the body.
Nearly every part of the body can be affected by cancerous cells, and they can then spread to other areas.
RISKS, SYMPTOMS AND TREATMENTS FOR LUNG CANCER, THE DEADLIEST CANCER IN THE WORLD
Prostate cancer is a type of cancer found in men that begins in the prostate gland and can then grow beyond that in more severe cases.
"The most common symptom is no symptom at all," Dr. Christopher Anderson, a urologist with New York-Presbyterian/Columbia University Irving Medical Center, previously told Fox News Digital in 2017.
Some men may experience symptoms such as pain in their bones and weight loss when the cancer has already spread, Anderson said.
Dr. Philip Kantoff, a medical oncologist and chair of the department of medicine at Memorial Sloan Kettering Cancer Center, reiterated that the disease does not typically cause symptoms.
Symptoms could instead be due to an enlarged or inflamed prostate, neither of which are cancerous.
Dr. Ketan Badani, vice chairman of urology at Mount Sinai Health System, said that "some patients may have vague urinary complaints," like having to urinate more frequently, and that there are no symptoms until the disease is advanced.
The majority of men who have urinary issues do not have prostate cancer, he noted.
Men ages 60 to 74 are considered more at risk, according to the Surveillance, Epidemiology and End Results (SEER) program.
Family history, "especially a first-degree relative like a father or brother" who has been diagnosed, is another concern, Badani added.
African, Afro-Caribbean, South Asian and Hispanic men are more at risk for "more aggressive" forms of prostate cancer, he said.
For men of African descent, there is an increased risk of both prostate cancer diagnosis and dying from prostate cancer, Anderson said.
There are several lifestyle changes men can implement into their lives to potentially reduce their risk of prostate cancer. This includes maintaining a healthy weight, staying active and having a healthy diet, according to the ACS, such as one including very little red and processed meat and processed foods, but filled with lots of fruits, vegetables and whole grains.
Most commonly, prostate cancer is adenocarcinomas, meaning it develops in the gland cells, according to ACS.
There are other types of prostate cancer, according to the source, but these are rare.
CLICK HERE TO SIGN UP FOR OUR LIFESTYLE NEWSLETTER
Other types are small cell carcinoma, neuroendocrine tumors, transitional cell carcinomas and sarcomas.
In general, prostate cancer grows very slowly.
Many people who have it die from other causes without ever knowing that they had the cancer, according to the ACS.
Prostate cancer is curable, so long as it's diagnosed early enough, according to Mayo Clinic.
Treatment options will depend on the stage of the cancer and the overall health of the individual. For early prostate cancer, immediate treatment may not be needed, per the source.
More severe cases of cancer are usually treated through radiation or surgery.
"A discussion with your physician is warranted before symptoms occur," Kantoff advised, adding that men should decide with their doctors if a prostate-specific antigen (PSA) test, which looks at the level of PSA in blood, is right for them.
For more Health articles, visit www.foxnews.com/health
Badani recommended that men receive both annual digital rectal exams and PSA tests. Multiple PSA tests over time are a better indicator of potential concerns as opposed to a single test result, he explained.
If you are concerned you might have prostate cancer, speak to an internal medicine doctor or a urologist, Anderson recommended. He stressed that all patients with blood in their urine should see a urologist.
PSA screening has been a controversial topic in the past. In 2012, the U.S. Preventative Services Task Force recommended against PSA screening when it said "there is moderate certainty that the benefits of PSA-based screening for prostate cancer do not outweigh the harms."
In 2018, the task force said in its final recommendation that men ages 55 to 69 should discuss potential benefits and negatives of a PSA screening with their physician before undergoing the test.
While a PSA screening has the potential to reduce the risk of death, negatives listed by the task force include "false-positive results that require additional testing and possible prostate biopsy; overdiagnosis and overtreatment; and treatment complications, such as incontinence and erectile dysfunction."
They do not recommend PSA screening in men ages 70 and above.
"Proper use of PSA is what I recommend from an early detection standpoint," Kantoff said.
Symptoms should not be the motivating factor for screening, he said, saying it should instead be a decision in one’s 40s about whether PSA testing should be done. He recommended that those with a family history or people of African American descent think about early detection.
An analysis of previous clinical trials published in 2017 said screening lessened the risk of dying from prostate cancer by 25 to 32% compared to men who did not get screened, a summary for patients explains online.
The Associated Press contributed reporting, as did Andy Sahadeo and Zoe Szathmary.
1 year 10 months ago
prostate-cancer, mens-health, Cancer, Health, lifestyle, medical-tech, health-care
Dad of two battling stage-four bone cancer - Jamaica Star Online
Dad of two battling stage-four bone cancer
Jamaica Star Online
1 year 10 months ago
News Archives - Healthy Caribbean Coalition
Civil Society Organisations Call for Octagonal Front of Package Warning Labelling Amidst Regional Vote!
CARICOM Member States are once again voting on the adoption of the Final Draft CARICOM Regional Standard for labelling pre-packaged foods (FDCRS 5:2010). This Standard includes octagonal warning labels on the front of packaged products to help individuals quickly, easily and correctly identify foods high in sugars, sodium or fats quickly.
This evidence-based strategy is known to support consumers in making healthier choices, aiming to combat non-communicable diseases, overweight, and obesity.
In a collaborative effort, the Healthy Caribbean Coalition (HCC), comprising local civil society organisations and allies, orchestrated a regional Call to Action on Saturday, September 16th, at 11:00 AM AST/10:00 AM JA time across several CARICOM territories, including Antigua and Barbuda, Barbados, The Bahamas, Belize, Dominica, Grenada, Jamaica, St. Lucia and St. Vincent and the Grenadines. Civil Society Organisations in St. Kitts and Nevis and Trinidad and Tobago supported the effort virtually.
The event highlighted regional civil society organisation support for the High In octagonal warning labels across the Caribbean and garnered the public’s perspectives on the implementation of High In front of package nutrition warning labelling across the Caribbean. This call to action served as a reminder to CARICOM leaders that they have committed to fast-tracking policies to address obesity in children and more broadly, tackling unhealthy food environments and NCDs.
After its successful adoption in Chile, octagonal Front of Package Warning Labelling (FOPWL) has been subsequently introduced in Peru (2019), Mexico (2020), and Uruguay (2020). Chile saw decreases in household volume of high-sweetened beverages and general products with ‘high-in’ labels. In Mexico, octagonal warning labels are projected to reduce caloric intake by 14.7% over five years, potentially saving the country an estimated US$1.8 billion in obesity-related costs.[1] It’s important to note that FOPWL does not harm trade; any short-term costs are outweighed by long-term health benefits and healthcare savings. Studies conducted by the Ministry of Health and Wellness in Jamaica,[2] PAHO[3] and other partners have shown that the octagonal High In warning label system effectively aids consumers in identifying products with excessive critical nutrients, which, when consumed excessively, raise the risk of overweight, obesity, and NCDs. Recent research by the University of the West Indies and PAHO, the first of its kind in the Caribbean, also underscores the substantial health and economic impact of octagonal warning labels by revealing that these labels could prevent 16% of NCD-related deaths in Barbados, potentially saving USD 732.8 million.[4]
The implementation of this labelling system aligns with CARICOM mandates, including the 2007 Port of Spain Declaration, the Communiqués of the 37th and 39th Conference of Heads of State and Government, the CARPHA 6-point policy package addressing obesity, and the PAHO Plan of Action for Obesity Prevention in Children and Adolescents. If the Standard is approved and endorsed, the Caribbean will join a growing number of countries that use the octagonal warning label regulations to combat obesity and NCDs, and ultimately protect the rights of their citizens to know what is in their food.
[1] Predicting obesity reduction after implementing warning labels in Mexico: A modeling study: https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1...
[[2] Superior Efficacy of Front-of-Package Warning Labels in Jamaica: https://iris.paho.org/handle/10665.2/53328
[[3] White-Barrow V, Gomes FS, Eyre S, et alEffects of front-of-package nutrition labelling systems on understanding and purchase intention in Jamaica: results from a multiarm randomised controlled trialBMJ Open 2023;13:e065620. doi: 10.1136/bmjopen-2022-065620
[4] Front-of-package warning labels save lives and resources: results from a modeling study in Barbados: https://iris.paho.org/handle/10665.2/57989
The post Civil Society Organisations Call for Octagonal Front of Package Warning Labelling Amidst Regional Vote! appeared first on Healthy Caribbean Coalition.
1 year 10 months ago
News
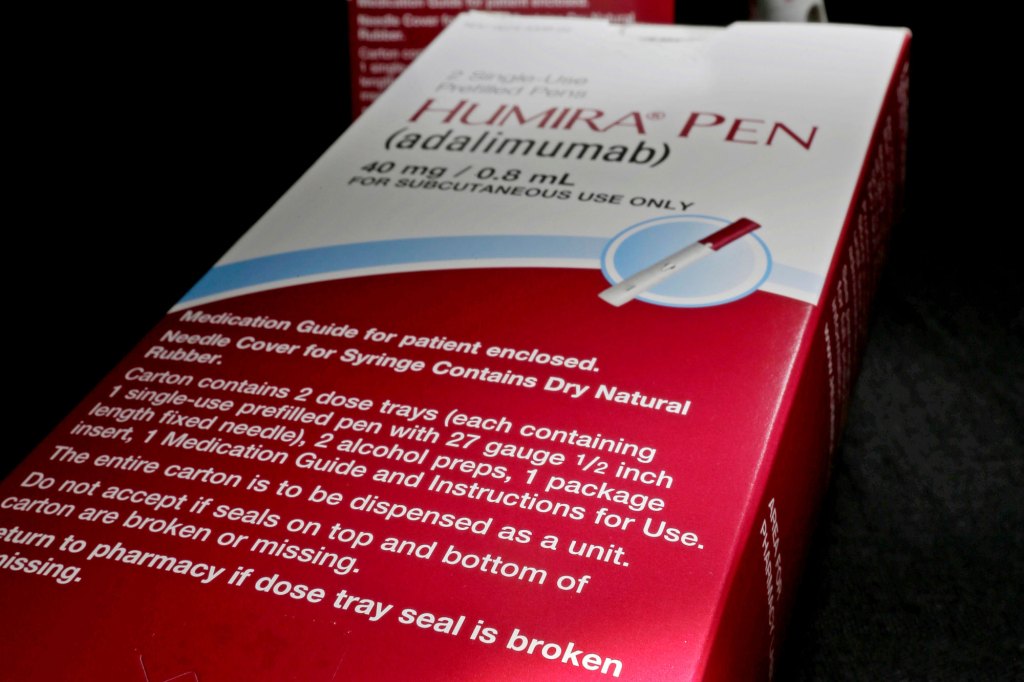
Save Billions or Stick With Humira? Drug Brokers Steer Americans to the Costly Choice
Tennessee last year spent $48 million on a single drug, Humira — about $62,000 for each of the 775 patients who were covered by its employee health insurance program and receiving the treatment. So when nine Humira knockoffs, known as biosimilars, hit the market for as little as $995 a month, the opportunity for savings appeared ample and immediate.
But it isn’t here yet. Makers of biosimilars must still work within a health care system in which basic economics rarely seems to hold sway.
For real competition to take hold, the big pharmacy benefit managers, or PBMs, the companies that negotiate prices and set the prescription drug menu for 80% of insured patients in the United States, would have to position the new drugs favorably in health plans.
They haven’t, though the logic for doing so seems plain.
Humira has enjoyed high-priced U.S. exclusivity for 20 years. Its challengers could save the health care system $9 billion and herald savings from the whole class of drugs called biosimilars — a windfall akin to the hundreds of billions saved each year through the purchase of generic drugs.
The biosimilars work the same way as Humira, an injectable treatment for rheumatoid arthritis and other autoimmune diseases. And countries such as the United Kingdom, Denmark, and Poland have moved more than 90% of their Humira patients to the rival drugs since they launched in Europe in 2018. Kaiser Permanente, which oversees medical care for 12 million people in eight U.S. states, switched most of its patients to a biosimilar in February and expects to save $300 million this year alone.
Biologics — both the brand-name drugs and their imitators, or biosimilars — are made with living cells, such as yeast or bacteria. With dozens of biologics nearing the end of their patent protection in the next two decades, biosimilars could generate much higher savings than generics, said Paul Holmes, a partner at Williams Barber Morel who works with self-insured health plans. That’s because biologics are much more expensive than pills and other formulations made through simpler chemical processes.
For example, after the first generics for the blockbuster anti-reflux drug Nexium hit the market in 2015, they cost around $10 a month, compared with Nexium’s $100 price tag. Coherus BioSciences launched its Humira biosimilar, Yusimry, in July at $995 per two-syringe carton, compared with Humira’s $6,600 list price for a nearly identical product.
“The percentage savings might be similar, but the total dollar savings are much bigger,” Holmes said, “as long as the plan sponsors, the employers, realize the opportunity.”
That’s a big if.
While a manufacturer may need to spend a few million dollars to get a generic pill ready to market, makers of biosimilars say their development can require up to eight years and $200 million. The business won’t work unless they gain significant market share, they say.
The biggest hitch seems to be the PBMs. Express Scripts and Optum Rx, two of the three giant PBMs, have put biosimilars on their formularies, but at the same price as Humira. That gives doctors and patients little incentive to switch. So Humira remains dominant for now.
“We’re not seeing a lot of takeup of the biosimilar,” said Keith Athow, pharmacy director for Tennessee’s group insurance program, which covers 292,000 state and local employees and their dependents.
The ongoing saga of Humira — its peculiar appeal to drug middlemen and insurers, the patients who’ve benefited, the patients who’ve suffered as its list price jumped sixfold since 2003 — exemplifies the convoluted U.S. health care system, whose prescription drug coverage can be spotty and expenditures far more unequal than in other advanced economies.
Biologics like Humira occupy a growing share of U.S. health care spending, with their costs increasing 12.5% annually over the past five years. The drugs are increasingly important in treating cancers and autoimmune diseases, such as rheumatoid arthritis and inflammatory bowel disease, that afflict about 1 in 10 Americans.
Humira’s $200 billion in global sales make it the best-selling drug in history. Its manufacturer, AbbVie, has aggressively defended the drug, filing more than 240 patents and deploying legal threats and tweaks to the product to keep patent protections and competitors at bay.
The company’s fight for Humira didn’t stop when the biosimilars finally appeared. The drugmaker has told investors it doesn’t expect to lose much market share through 2024. “We are competing very effectively with the various biosimilar offerings,” AbbVie CEO Richard Gonzalez said during an earnings call.
How AbbVie Maintains Market Share
One of AbbVie’s strategies was to warn health plans that if they recommended biosimilars over Humira they would lose rebates on purchases of Skyrizi and Rinvoq, two drugs with no generic imitators that are each listed at about $120,000 a year, according to PBM officials. In other words, dropping one AbbVie drug would lead to higher costs for others.
Industry sources also say the PBMs persuaded AbbVie to increase its Humira rebates — the end-of-the-year payments, based on total use of the drug, which are mostly passed along by the PBMs to the health plan sponsors. Although rebate numbers are kept secret and vary widely, some reportedly jumped this year by 40% to 60% of the drug’s list price.
The leading PBMs — Express Scripts, Optum, and CVS Caremark — are powerful players, each part of a giant health conglomerate that includes a leading insurer, specialty pharmacies, doctors’ offices, and other businesses, some of them based overseas for tax advantages.
Yet challenges to PBM practices are mounting. The Federal Trade Commission began a major probe of the companies last year. Kroger canceled its pharmacy contract with Express Scripts last fall, saying it had no bargaining power in the arrangement, and, on Aug. 17, the insurer Blue Shield of California announced it was severing most of its business with CVS Caremark for similar reasons.
Critics of the top PBMs see the Humira biosimilars as a potential turning point for the secretive business processes that have contributed to stunningly high drug prices.
Although list prices for Humira are many times higher than those of the new biosimilars, discounts and rebates offered by AbbVie make its drug more competitive. But even if health plans were paying only, say, half of the net amount they pay for Humira now — and if several biosimilar makers charged as little as a sixth of the gross price — the costs could fall by around $30,000 a year per patient, said Greg Baker, CEO of AffirmedRx, a smaller PBM that is challenging the big companies.
Multiplied by the 313,000 patients currently prescribed Humira, that comes to about $9 billion in annual savings — a not inconsequential 1.4% of total national spending on pharmaceuticals in 2022.
The launch of the biosimilar Yusimry, which is being sold through Mark Cuban’s Cost Plus Drugs pharmacy and elsewhere, “should send off alarms to the employers,” said Juliana Reed, executive director of the Biosimilars Forum, an industry group. “They are going to ask, ‘Time out, why are you charging me 85% more, Mr. PBM, than what Mark Cuban is offering? What is going on in this system?’”
Cheaper drugs could make it easier for patients to pay for their drugs and presumably make them healthier. A KFF survey in 2022 found that nearly a fifth of adults reported not filling a prescription because of the cost. Reports of Humira patients quitting the drug for its cost are rife.
Convenience, Inertia, and Fear
When Sue Lee of suburban Louisville, Kentucky, retired as an insurance claims reviewer and went on Medicare in 2017, she learned that her monthly copay for Humira, which she took to treat painful plaque psoriasis, was rising from $60 to $8,000 a year.
It was a particularly bitter experience for Lee, now 81, because AbbVie had paid her for the previous three years to proselytize for the drug by chatting up dermatology nurses at fancy AbbVie-sponsored dinners. Casting about for a way to stay on the drug, Lee asked the company for help, but her income at the time was too high to qualify her for its assistance program.
“They were done with me,” she said. Lee went off the drug, and within a few weeks the psoriasis came back with a vengeance. Sores covered her calves, torso, and even the tips of her ears. Months later she got relief by entering a clinical trial for another drug.
Health plans are motivated to keep Humira as a preferred choice out of convenience, inertia, and fear. While such data is secret, one Midwestern firm with 2,500 employees told KFF Health News that AbbVie had effectively lowered Humira’s net cost to the company by 40% after July 1, the day most of the biosimilars launched.
One of the top three PBMs, CVS Caremark, announced in August that it was creating a partnership with drugmaker Sandoz to market its own cut-rate version of Humira, called Hyrimoz, in 2024. But Caremark didn’t appear to be fully embracing even its own biosimilar. Officials from the PBM notified customers that Hyrimoz will be on the same tier as Humira to “maximize rebates” from AbbVie, Tennessee’s Athow said.
Most of the rebates are passed along to health plans, the PBMs say. But if the state of Tennessee received a check for, say, $20 million at the end of last year, it was merely getting back some of the $48 million it already spent.
“It’s a devil’s bargain,” said Michael Thompson, president and CEO of the National Alliance of Healthcare Purchaser Coalitions. “The happiest day of a benefit executive’s year is walking into the CFO’s office with a several-million-dollar check and saying, ‘Look what I got you!’”
Executives from the leading PBMs have said their clients prefer high-priced, high-rebate drugs, but that’s not the whole story. Some of the fees and other payments that PBMs, distributors, consultants, and wholesalers earn are calculated based on a drug’s price, which gives them equally misplaced incentives, said Antonio Ciaccia, CEO of 46Brooklyn, a nonprofit that researches the drug supply chain.
“The large intermediaries are wedded to inflated sticker prices,” said Ciaccia.
AbbVie has warned some PBMs that if Humira isn’t offered on the same tier as biosimilars it will stop paying rebates for the drug, according to Alex Jung, a forensic accountant who consults with the Midwest Business Group on Health.
AbbVie did not respond to requests for comment.
One of the low-cost Humira biosimilars, Organon’s Hadlima, has made it onto several formularies, the ranked lists of drugs that health plans offer patients, since launching in February, but “access alone does not guarantee success” and doesn’t mean patients will get the product, Kevin Ali, Organon’s CEO, said in an earnings call in August.
If the biosimilars are priced no lower than Humira on health plan formularies, rheumatologists will lack an incentive to prescribe them. When PBMs put drugs on the same “tier” on a formulary, the patient’s copay is generally the same.
In an emailed statement, Optum Rx said that by adding several biosimilars to its formularies at the same price as Humira, “we are fostering competition while ensuring the broadest possible choice and access for those we serve.”
Switching a patient involves administrative costs for the patient, health plan, pharmacy, and doctor, said Marcus Snow, chair of the American College of Rheumatology’s Committee on Rheumatologic Care.
Doctors’ Inertia Is Powerful
Doctors seem reluctant to move patients off Humira. After years of struggling with insurance, the biggest concern of the patient and the rheumatologist, Snow said, is “forced switching by the insurer. If the patient is doing well, any change is concerning to them.” Still, the American College of Rheumatology recently distributed a video informing patients of the availability of biosimilars, and “the data is there that there’s virtually no difference,” Snow said. “We know the cost of health care is exploding. But at the same time, my job is to make my patient better. That trumps everything.”
“All things being equal, I like to keep the patient on the same drug,” said Madelaine Feldman, a New Orleans rheumatologist.
Gastrointestinal specialists, who often prescribe Humira for inflammatory bowel disease, seem similarly conflicted. American Gastroenterological Association spokesperson Rachel Shubert said the group’s policy guidance “opposes nonmedical switching” by an insurer, unless the decision is shared by provider and patient. But Siddharth Singh, chair of the group’s clinical guidelines committee, said he would not hesitate to switch a new patient to a biosimilar, although “these decisions are largely insurance-driven.”
HealthTrust, a company that procures drugs for about 2 million people, has had only five patients switch from Humira this year, said Cora Opsahl, director of the Service Employees International Union’s 32BJ Health Fund, a New York state plan that procures drugs through HealthTrust.
But the biosimilar companies hope to slowly gain market footholds. Companies like Coherus will have a niche and “they might be on the front end of a wave,” said Ciaccia, given employers’ growing demands for change in the system.
The $2,000 out-of-pocket cap on Medicare drug spending that goes into effect in 2025 under the Inflation Reduction Act could spur more interest in biosimilars. With insurers on the hook for more of a drug’s cost, they should be looking for cheaper options.
For Kaiser Permanente, the move to biosimilars was obvious once the company determined they were safe and effective, said Mary Beth Lang, KP’s chief pharmacy officer. The first Humira biosimilar, Amjevita, was 55% cheaper than the original drug, and she indicated that KP was paying even less since more drastically discounted biosimilars launched. Switched patients pay less for their medication than before, she said, and very few have tried to get back on Humira.
Prescryptive, a small PBM that promises transparent policies, switched 100% of its patients after most of the other biosimilars entered the market July 1 “with absolutely no interruption of therapy, no complaints, and no changes,” said Rich Lieblich, the company’s vice president for clinical services and industry relations.
AbbVie declined to respond to him with a competitive price, he said.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 10 months ago
Health Care Costs, Health Industry, Pharmaceuticals, Drug Costs, Kentucky, New York, Prescription Drugs, Tennessee
Tea Tree Oil for Hair: Benefits, Uses, and Products - Prevention Magazine
- Tea Tree Oil for Hair: Benefits, Uses, and Products Prevention Magazine
- 10 oils for hair growth Jamaica Observer
- 5 essential oils to boost hair growth Hindustan Times
- View Full Coverage on Google News
1 year 10 months ago
Novel botanical lotion may improve aging skin on arms, thighs of women
A novel firming and toning body lotion containing bioactive botanicals may improve upper arm firmness and thigh cellulite in women, according to a study.“A large proportion of research and clinical attention in aesthetic medicine is devoted to the restoration and repair of age-related changes in the skin,” Elizabeth T.
Makino, BS, CCRA, MBA, of SkinMedica, Allergan Aesthetics, an AbbVie Company, and colleagues wrote. “In recent years, these efforts have increasingly expanded into the care of body skin, broadening the field’s historical near-exclusive focus on the face
1 year 10 months ago
Watch: Thinking Big in Public Health, Inspired by the End of Smallpox
One of humanity’s greatest triumphs is the eradication of smallpox. Many doctors and scientists thought it was impossible to eliminate a disease that had been around for millennia and killed nearly 1 in 3 people infected. Smallpox is the first and only human disease to be wiped out globally.
KFF Health News held a web event Thursday that discussed how the lessons from the victory over smallpox could be applied to public health challenges today. The online conversation was led by Céline Gounder, physician-epidemiologist and host of “Eradicating Smallpox,” Season 2 of the Epidemic podcast.
Gounder was joined by:
Helene Gayle, a physician and epidemiologist, is president of Spelman College. She is a board member of the Bill & Melinda Gates Foundation and past director of the foundation’s HIV, tuberculosis, and reproductive health program. She spent two decades with the Centers for Disease Control and Prevention focusing primarily on HIV/AIDS prevention and global health.
William “Bill” Foege was a leader in the campaign to end smallpox during the 1970s. An epidemiologist and physician, Foege led the CDC from 1977 to 1983. He appears in the virtual learning series “Becoming Better Ancestors: Applying the Lessons Learned from Smallpox Eradication.” Foege is featured in Episode 2 of the “Eradicating Smallpox” docuseries.
click to open the transcript
Transcript: Thinking Big in Public Health, Inspired by the End of Smallpox
Note: This transcript was generated by a third-party site and may contain errors. Please use the transcript as a tool but check the corresponding audio before quoting the web event.
TRANSCRIPT
[The video trailer for season 2 of the Epidemic podcast, “Eradicating Smallpox,” begins to play]
Céline Gounder: Bangladesh 50 years ago, we were on the cusp of something big, something we had never done before. We were about to wipe smallpox off the planet. It’s one of humanity’s greatest triumphs. One public health has yet to repeat. I’m Dr. Celine Gounder. I’m a physician and epidemiologist.
This season of Epidemic, we’re going to India and Bangladesh, where smallpox made its last stand, to understand how health workers beat the virus. The question I’m asking, “How can we dream big in public health again?” From KFF Health News and just human productions, Epidemic, eradicating smallpox. Listen wherever you get your podcasts.
[Video trailer ends]
Céline Gounder: Good morning everyone, and thanks for joining us today. I’m Dr. Celine Gounder. I’m editor-at-large for Public Health at KFF Health News and I’m the host of the Epidemic Podcast. In today’s conversation, we’re going to talk about lessons to be learned from the eradication of smallpox and how those can be applied to public health challenges today. The eradication of smallpox is one of humanity’s greatest triumphs. Many doctors and scientists thought it was impossible to eliminate a disease that had lasted for millennia and killed nearly one in three people infected. Smallpox remains the first and only human disease to be wiped out globally.
Just a few logistical details before we get started. The briefing is being recorded and the link to the recorded version will be emailed to everyone later today. We also have ASL interpretation available. To access it, please click on the globe icon in your Zoom control panel and select ‘American Sign Language.’ A screen will appear and you will be able to view the interpreter. Questions should be entered using the Q&A function on Zoom and can be sent in during the discussion.
I’d like to move forward with introducing our panelists today. Dr. Bill Foege is an epidemiologist and physician and was a leader in the campaign to end smallpox during the 1970s. Foege is featured in episode two of the Eradicating Smallpox docuseries, and he’s also featured in the Nine Lessons series produced by the Becoming Better Ancestors Project. The Nine Lessons, available at ninelessons.org, is a virtual learning series about how the lessons from smallpox eradication could be applied to COVID and other public health and societal challenges.
Also, joining us today is Dr. Helene Gayle, who’s also an epidemiologist and physician. She’s the president of Spelman College. She’s also a board member of the Bill & Melinda Gates Foundation and past director of the Foundation’s program on HIV, Tuberculosis and reproductive health. She spent two decades with the Centers for Disease Control and Prevention, focusing primarily on HIV AIDS prevention and Global Health.
So welcome and thank you for joining us today, Bill and Helene. I’d like to start with talking about some of the challenges we face in science communication. And as we’ve seen during the COVID pandemic, one of the big challenges is balancing reassurance with uncertainty. And before I ask you my questions, I’m going to play a clip of Dr. Tony Fauci speaking about this as part of the Nine Lessons series. So let’s give that a listen.
[Video clip from the Nine Lessons series begins to play]
Tony Fauci: If you have a static situation with nothing changing and you get one opinion one day, and then a week later you change, that’s flip-flopping. When you have a dynamic situation that’s evolving week to week and month to month, as a scientist, to be true to yourself and to be true to the discipline of science, you have to collect data as the situation evolves, which almost invariably will necessitate your changing policy, changing guidelines, changing opinion. And that’s exactly what happened with things like mask wearing. We didn’t know until weeks and weeks into the outbreak that a lot of the transmission was by people who were without symptoms. It was that that made the CDC and all of us say, “We really don’t need to be wearing masks.” As soon as we found out that, A, there was no shortage, B, we were getting good data, that outside of the hospital setting masks did work, and three, we found out that 50% of the infections were transmitted from someone who had no symptoms. When you put all those three things together, then the science tells us everybody should be wearing a mask.
[Video clip ends]
Céline Gounder: Bill, how did this play out in the smallpox eradication program, specifically this idea of scientific certainty, uncertainty, and science communication?
Bill Foege: This is actually a balance that goes far beyond public health and medicine and almost everything we do. And on the one hand, you have to have enough certainty in order to get other people to follow you. There’s a book by Gary Wills on Leadership, and it’s entitled Certain Trumpets. He takes this from the Bible verse that says, “If you hear an uncertain trumpet, who would gird for battle?”
So you have to have enough certainty. The other side of that though is Richard Feynman, the physicist who said, “Certainty is the Achilles heel of science.” If we believe something is true, we stop looking for other answers to why this is happening. And I think in smallpox, we always tried to present certainty in what we were doing. And all the time we worried about what could go wrong, what if we lose political support? I didn’t see HIV coming, but boy, if I had, that would’ve been a big problem to deal with.
Céline Gounder: Helene, don’t you think public health officials should still be confident in expressing, particularly in an emergency, what we know and their recommendations for managing a public health crisis, and how do you balance that confidence and reassurance with the lack of certainty?
Helene Gayle: So I think, and building on some of the things that Bill said, I think part of it is building the confidence in the communicator. And I think one of the things, and I point to Tony Fauci, is one of those people who I think Americans developed a sense of confidence with him because of his willingness and ability to say when we were wrong and what we know and when we knew it. And so I think recognizing that a lot of this is about building trust and building trust in the message as well as in the messenger. I think that’s where some of the ability to be confident, letting people know that you’re trying to give them the information as soon as you have it, but also being honest that this is evolving.
A message is just a slice in time. And I think it’s important that we remember that we’re creating a narrative every time we open our mouths and thinking about what’s the narrative that we’re creating and being consistent in that narrative. So I think the consistency, building that trust, being able to say what you know and what you don’t know is what really I think builds the confidence in the messages. I think what we saw through this pandemic as well, the COVID pandemic as well as past, are people who are unwilling to admit what they know and what they don’t know, unwilling to go back and explain why we said something when we said it and why we’re making that explanation of why we’re now changing, as I think Tony Fauci did very clearly about mask wearing.
So I think all of those things that really are about building trust and confidence are what can make us better in our communication as public health officials.
Céline Gounder: So it still amazes me that the global health community decided to take on smallpox eradication. We often hear about sustainability, cost-effectiveness, those kinds of economic concepts. What does it mean, Helene, for a program to be sustainable? And when we say sustainable, for whom?
Helene Gayle: Well, I think what we hope when we talk about sustainability is that efforts that are important for the short run can be sustained over the long run. And I think what we see so often in public health is that we have this massive surge of resources, personnel, effort, that then we let go of in between times.
So each time we have a pandemic, we have to create this big surge all over again. What we need in public health is to be able to have that kind of long-term, sustainable approach, understanding that there will be times when we have to have those surges, but not letting everything go in between time. When you say for whom, it’s really about how do we create a system and have a system that is in place that gets us not only at the times of great need and crisis, but is there for the public’s health for the long-term. And that’s what I hope we can move to as we think about public health in America and around the world.
Céline Gounder: Bill, does that sound like that’s a “sustainable goal” and should we be setting our public health goals based on what some think is sustainable or not?
Bill Foege: Well, sustainability is a problem that I often had because people require evidence of sustainability before they’ll fund something, but you don’t know what is sustainable until you try and do it. One of the lessons that I learned in the seventies was, in this country, the appropriations for measles would go up when there were lots of measles cases and they would go down when cases were reduced.
And inevitably, when they would go down, then the numbers had come up again. And so we had these variations. And we made a decision in the 1970s what would happen if we could interrupt transmission once, and that changes everything. Now the norm would be no transmission, and you could sustain the appropriations and it worked. We finally did that. So sustainability is something that bothers me. The pragmatists demand this, and I understand where they’re coming from, but there was a fellow by the name of Harlan Cleveland who was an American diplomat. He was our ambassador to NATO for many years. And late in his life, he became interested in global health and he was astonished at what happened with so few resources. And he came to the conclusion that global health workers are fueled on unwarranted optimism. And I like that phrase, because that is in fact what we do, is we become very optimistic and we make something happen that could not have been foreseen, that it would happen.
Céline Gounder: So this also reminds me about a conversation we had on the podcast with, believe it or not, a science fiction writer. Her name is adrienne maree brown, and we spoke with her about how she imagines world’s, possibilities different from our own. So let’s hear a short clip of that now.
Where do you find the inspiration to think up, to dream up the world’s that are so wildly different from our present reality?
[Audio clip from episode 1 of the “Eradicating Smallpox” begins to play]
adrienne maree brown: Saying that stuff is just the way it is. That’s one of the greatest ways that those who currently benefit from the way things are keep us from even imagining that things could be different. For centuries in this country, we were told that slavery was just the way things are and that it could never be any different. And yet there are people in those systems who said, “This isn’t right, this isn’t fair. Something else is actually possible.”
So a lot of the work of radical imagination, for me, is the work of saying, can we imagine a world in which our lives actually matter and we structure our society around the care that we can give to each other, the care that we need.
[Audio clip ends]
Céline Gounder: Bill, you just talked about unwarranted optimism and you told me once, in fact, I think more than once to bet on the optimist. But to go back to what you were saying about the pragmatist, doesn’t it make more sense on some level to be pragmatic and realistic if you want to get things done? And how would realism have gotten in the way of efforts to eradicate smallpox?
Bill Foege: Well, I think realism would have kept us from trying many things that we’ve tried. And the clip you just showed about an imagination that goes beyond realism is so important. If I would be director of CDC again, if I had a problem, I would try to get six comedians to come to CDC and I present them with the problem because they think in a different world than realism. And so I think it just makes sense to be unrealistic that we can do these things.
Céline Gounder: Helene, what about you? How did you balance thinking big versus being pragmatic when you were leading public health programs over the course of your career?
Helene Gayle: Well, I didn’t bring in comedians, but I think maybe I missed the boat on that. I love that idea. I like to think that I was able to combine the two. I think if you don’t think big, you will only achieve small progress. So I think you have to have big goals, but big goals can also be chunked into bite-sized pieces. So I think mixing the practical of what are the short-term games that are necessary to get to those big goals, both, give you a sense of what’s pragmatic and possible, but also keeps you inspired towards the bigger goal.
I think it’s also the case in public health where oftentimes we are operating with very difficult political situations. And again, sometimes you have to be the realist and understand what the limits are, but at the same time not give up on what’s your ultimate goal, what’s your ultimate vision, and keeping that front and center, it’s incredibly important, particularly as we think about how we inspire, back to the unwarranted optimism, how we inspire public health workers to keep going. People don’t get inspired by the short term, “Did I get my stock in today?” They get inspired by, “I’m part of eradicating a disease or stopping a pandemic.” So I think we have to combine the two.
Bill Foege: I might say that in India, we would have a meeting every month in the endemic states and go over what we had learned that month, and we would end the meeting by setting goals for the next month. We never once reached those goals until the last month. They were always beyond what we could do, but they gave us a vision of what we hoped we could do.
Céline Gounder: So this also reminds me of another aspect of goal setting. In another episode of the podcast, we spoke with a global health expert, Dr. Madhu Pai at McGill University, and he pointed out that historically it’s been white men in Europe and in the United States who’ve really driven the agenda in global health. Here’s just a short clip from Madhu.
[Audio clip from episode 2 of the “Eradicating Smallpox” begins to play]
Madhukar Pai: We need to flip the switch and recenter global health away from this, what I call default settings in global health, to the front lines. People on the ground, people who are Black, indigenous, people who are in communities, people who are actually dealing with the disease burden, people who are dying off it, people who have actually lived experience of these diseases that we’re talking about, having them run it is the most radical way of re imagining and shifting power and global health.
[Audio clip ends]
Céline Gounder: So Bill, who set the smallpox eradication goals? Was this local or global experts or both? Was it local communities and how were those different perspectives weighed and balanced in the program?
Bill Foege: Well, the global goal was set by WHO. It was originally conceived by the Soviet Union and presented to WHO, and it got only three votes the first time. Later, when the Soviet Union and the United States combined their efforts, they were able to convince the World Health Assembly and WHO took this on. So the global goal was set by WHO, but countries had the ability to say no. And Ethiopia went for a long time not becoming part of the program, they had other priorities. And these are legitimate priorities that World Bank once had a discussion on whether we should get into polio eradication or not. And I agreed to be part of the debate, even though I hate debates. I agreed to be part because I wanted to know what were the strongest arguments against polio eradication. And for me, there were two of them.
One was that this would distract from other global health efforts. People would focus on this. But the other one came from an African leader who said, “This is neocolonialism. You’re telling us how to spend our money on a disease problem and not allowing us to make that decision.” My counter to that was, “I understand that, but I also understand when Gandhi said his idea of the golden rule was that he should not be able to enjoy what other people could not enjoy.” And so I said, “If I can enjoy the fact that my children, my grandchildren, and now my great-grandchildren are free of polio, I have an obligation as a parent to share that with everyone.”
Céline Gounder: Helene, very often it’s scientific experts, physicians, epidemiologists who really lead the goal setting. Is there anything wrong with this technocratic approach to public health goal setting, and isn’t that just “following the science?”
Helene Gayle: Well, it’s obviously following the science at a macro level, but I think, while it’s important to set these global goals and these big overarching goals, it’s also very important to listen to the people whose health we’re actually trying to have an impact on. And I can remember, during the HIV pandemic, where once people realized how important it was to mobilize resources, there was an unprecedented amount of resources available for HIV, and we got from several countries around the world, the pushback just as Bill was talking about, because they said, “Malaria is a bigger problem for me. We have more people who die from malaria, from measles, from other infectious diseases. So where are our resources for the things that are making the biggest difference for our people?”
So I think it’s great to set the global goals and to be able to have these big overarching goals, but we can’t do that in the absence of also listening to the national and local needs and making sure that we’re thinking flexibly about how we use our resources so that what we do really meets the greatest needs of people on the ground.
Céline Gounder: Bill, you once quoted Einstein to me who said, “Perfection of means and confusion of goals seem, in my opinion, to characterize our age.” So are government officials and public health leaders somehow confused about public health goals while being overly focused on perfecting public health tools?
Bill Foege: I think so. You can’t stop scientists from trying to enlarge their area of knowledge. This is what scientists do. They try to figure out what is right and what is wrong. And so yes, we do confuse this. And it doesn’t matter whether you’re talking about a person, a state, a nation or the world, we devalue health until the day we lose it, and then suddenly it becomes so important. And so this idea of conveying what should happen ahead of time so we don’t lose health is problematic. But yes, it’s much easier to concentrate on the specifics and lose our sight of where we’re actually going with this.
Céline Gounder: Can you just give an example of this attempt to perfect a public health tool?
Bill Foege: Well, with vaccines, you see that people keep improving the vaccines, but don’t improve how to get them to everyone. The clip you showed on white people, mainly white men, making the decisions on global health in the past, is so true. And I’ve just finished reviewing the history of global health, and I think the one thing that was most destructive of global health was colonialism. Some people try to justify it on the basis of it brought new science and so forth, but just think of this country and the fact that colonialism killed off so many people that the slave trade became so important.
And so today, we’re still operating with the effects of colonialism in this hemisphere. Not seeing the vision of the big goal and concentrating on small things, it’s easier for all of us to do.
Céline Gounder: Helene, do you agree that public health officials are confused about the goals? And if so, why and how?
Helene Gayle: Well, I think it’s hard to talk about public health officials as a monolith, and it’s part of the challenge, particularly in this country, is that we have such a disjointed public health system. And I think we would benefit from having a much different public health system, such that people can individualize their roles, what they want to focus on, et cetera. But at a national level, and I would argue even at the global level, that there is a system that is consistent about what’s most important and what’s most important to deliver on.
So I do think that there’s a lot of inconsistency in our system. I think we have a fragmented public health system, and we would really benefit by having something that really had a much more of a network that is coordinated than what we have today.
Céline Gounder: I just got back actually from vacation in Morocco and I happened to be staying in the Medina in Marrakesh the night of the earthquake. And it’s now been estimated that nearly 3,000 people have died in that earthquake or from that earthquake, to date. I felt it, but the building where I was staying sustained hardly any damage. And to date, I haven’t heard of any tourists or expats having been reported dead or seriously injured. Now, this was not an infectious disease outbreak, but it is a public health crisis of a kind, and some are more likely to be hurt and die than others. What does this tell us about, Bill, how to build resilience into the system and how was this done in the context of smallpox?
Bill Foege: Well, the resilience is a difficult thing because we think locally. Well, wherever you are in the world, you’re both local and global. So I keep telling students, wherever you’re working, you’re working on global health. And so start thinking that way of how do we incorporate all these people. And see, you’re absolutely right. It doesn’t take an infectious disease. It takes a disaster to show what the social problems are that are causing this. Michael Osterholm once said, “One of the best fire departments we have is at the Minneapolis airport.” He said, “If we go 10 years or 15 years without a crash, no one will reduce their budget.” This is the kind of resilience that we need in public health. The last appropriations hearing that I had as director of CDC was chaired by Senator Hatfield from Oregon. He was the chair of the entire Appropriations Committee, but he asked permission, as a favor to me, to actually share this last one.
He asked me a question that I was not expecting, which is the one you just asked. He asked, “If you were in charge, how would you improve the sustainability of public health?” And I told him that there were three things I would do. Number one, I would identify any program that has a positive benefit cost ratio, that is, for a dollar invested, you save more than a dollar, plus you improve health. Because if you don’t do that, you’re agreeing to spend money and have the disease both. And I said, “If you took these programs,” and I said, “In order to avoid infighting between the Congress and the executive branch, I put this totally in charge of Congress.” You decide when a program has a positive benefit cost ratio. And now it doesn’t compete with other things in the budget, it becomes something that’s an entitlement. We need this because it is cheaper and it improves health.
Number two, I said, “I would index public health to healthcare expenditures, because the ratio of public health to healthcare keeps going down every year.” I said, “I would accept whatever it is right now and say we have to index our public health spending to that.”
And the third, I would come up with mechanisms to improve and reward programs that benefit outcomes. Today, we benefit access and process, but not outcomes. And so, if we could benefit outcomes, it would change the way the insurance companies work and other programs work. So those three things I think would provide sustainability and public health we don’t have now.
Céline Gounder: Helene, how was resilience built into the system in the context of HIV and or TB?
Helene Gayle: I’ll answer that in a minute, but I just want to add on and taking from the example that you gave from Morocco that I think in many cases we’re talking about sustainability and resilience, but we’re also talking about equity. At the end of the day, the reason you probably were less likely to get impacted was you were probably staying in a building where the construction had been done in a way that it was as sustainable and not prone to the conditions of earthquake. And the people who are likely to have lost their lives were probably living in substandard building situations. So I think every time we think about sustainability and resilience, we also have to think about equity and are we making sure that the way in which we design our programs take equity into consideration, because that’s ultimately what is going to make populations and people have the kind of resilience that’s necessary.
I think when I look at the programs like tuberculosis and HIV, I think what we tried to really do was to build up systems as we went along, because the best way to make sure that our efforts were sustainable and had resilience built into them was to actually build systems, not just focus on the program or the effort that we were doing.
So in HIV, clearly when I look back on the public health infrastructure that was built, the human capacity that was developed as a result of HIV, that’s what starts building in resilience because you’re not just building for the HIV pandemic, but you’re really using those dollars in ways that can help to strengthen systems. And that’s what I think we have the kind of resilience and sustainability that we’re talking about.
Céline Gounder: Lately, I’ve been thinking a lot about this concept of “Wicked problems.” And for people who are not familiar with this term, it goes back to the management literature several decades ago. And these are complicated, they’re messy, they’re context specific problems. People may not agree that there is a problem or what the problem is, they disagree on what caused it. And with wicked problems, there’s no one right solution, just some that might be less bad, might often create new problems. And so, these are very much about values and not just science. Bill, how would you apply this idea of wicked problems to public health challenges like smallpox or COVID?
Bill Foege: Well, wicked problems turns out to be a good expression of, a great picture of this. And when I think of vaccines, for instance, in the beginning, in 1796 of the smallpox vaccine, and how they’ve improved in numbers and types, when I was born, my baby book shows I have got only two vaccinations. Children today will get 18 or 19 or 20 different vaccinations. And you look at the future of this, we now have two vaccines against cancer, one against liver cancer and one against cervical cancer. We’re going to see more vaccines against neoplasms. You look at the possibility of having vaccines in the future for certain heart diseases or even for addiction, alcoholism and drug addiction, and the possibilities are so great. And yet at the same time, we have more and more people who don’t trust science, don’t trust government, and they become anti-vaxxers.
So this is the real challenge of vaccines. It will continue to be the foundation of global health, but we have to figure out how to get people incorporated in the solutions. Vashon Island in Puget Sound had a reputation for very low immunization uptake, and many of the people on the island were the hippies of the sixties and they didn’t trust government and so forth. The New York Times actually had a front page article on the rate of immunization in children, and I think about 19% were not being immunized.
Now, they would not listen to the health officers of Seattle or anyone else of authority coming in, but two parents who had been Peace Corps volunteers started their own program of finding out from people what would it take for you to change your mind. What is it that you don’t know that you wish you knew? The vaccination rate decreased from 81%, or increased from 81% up to 88%, 89%. They were doing something at a grassroots level that we could not have done from the top down. And so, there are solutions to wicked problems, but they sure do require energy and organization and the ability to respect culture.
Céline Gounder: Helene, is there a way we can better align people who have different sets of values around some of the same public health goals or strategies when it comes to some of these wicked problems, whether that is COVID or some of the other problems facing us today, whether it may be climate change or disinformation. Bill mentioned some of the challenges with anti-vaxxers and anti-science.
Helene Gayle: Well, this is another time where I think we should bring in the comedians, but I do think, maybe not the comedians, but to take a point from what you were saying earlier, Bill, I do think looking at how do you find the common ground? And sometimes there’s only 5% of common ground, but you can start with that and continue to grow from there. I think oftentimes, we approach these things that are adversarial in a counter adversarial way. So if somebody’s hostile, we up the hostility, instead of thinking, “All right, where can we find common ground? What are the things that we all agree upon?”
And sometimes it’s just the simple fact that we agree that saving lives is a high value and you can start from there and begin to develop the proof points that make nonbelievers believers. So I think we don’t do enough of thinking about where we find common ground, and instead, go to our corners and think by continuing to insist on what we believe and think that that’s what’s going to convince people, versus starting from where we all have a common belief and building from there. I don’t know any other way to do it. It’s not a magic bullet. It won’t work all the time. But I also think there has to be a point at which you recognize there are some people who you will never get on your side, and if you continue to try to wait for that to happen, you’ll get stuck and not move forward.
So there’s always a certain point when you just need to keep moving forward, understanding that if you demonstrate effectiveness, that may be the most likely way of bringing others along.
Bill Foege: When I’ve had an opportunity to meet with anti-vaxxers, I always start with the fact that I know no parent does this, withholding vaccines, to hurt their child.
Helene Gayle: Exactly.
Bill Foege: They do it only because they believe it’s the best thing for their child. And so if you can start there, you’re in a different position than if you just say, “Well, don’t you read the literature? Don’t you listen to…?” So I think understanding that there’s a reason why people feel this way is the beginning.
Céline Gounder: So earlier we were talking a bit about public health tools and this desire to perfect public health tools, but at the same time, innovations in medical technology were in fact key to eradicating smallpox, especially a simple little tool called the bifurcated needle. Here’s a clip of some smallpox eradication workers discussing this tool from episode four of the podcast.
In the early 1970s, smallpox was still stalking parts of South Asia. India had launched its eradication program more than a decade before, but public health workers couldn’t keep up with the virus. Enter the bifurcated needle.
[Audio clip from episode 4 of the “Eradicating Smallpox” podcast begins to play]
Tim Miner: It was a marvelous invention. In its simplicity, it looks like a little cocktail fork.
Céline Gounder: You dip the prongs into a bit of vaccine.
Tim Miner: And you would just prick the skin about 12 or 15 times until there was a little trace of blood, and then you’d take another one.
Céline Gounder: It barely took 30 seconds to vaccinate someone. And it didn’t hurt.
Yogesh Parashar: No.
Céline Gounder: Well, it didn’t hurt too much.
Yogesh Parashar: It was just like a pin prick rapidly done on your forearm. You had a huge supply with you and you just went about and dot, dot, dot, vaccinated people. Carry hundreds with you at one go.
Tim Miner: And you could train somebody in a matter of minutes to do it.
Céline Gounder: Easy to use, easy to clean, and a big improvement over the twisting teeth of the vaccine instrument health workers had to use before. The bifurcated needle was maybe two and a half, three inches long, small but sturdy enough for rough-and-tumble field work.
Yogesh Parashar: It was made of steel, and it used to come in something that looked like a brick. It was just like one of those gold bricks that you see in the movies.
Céline Gounder: And maybe worth its weight in gold.
[Audio clip ends]
Céline Gounder: So, Bill, public health officials say, in the context of COVID, that we now have the tools to diagnose and treat and prevent COVID, but are these tools enough for us to declare victory over COVID when not everyone has access to those tools? And in the context of smallpox, how did non-biomedical tools compliment biomedical innovations like the bifurcated needle?
Bill Foege: Well, going back to what Helene said, we have to be thinking of this globally and everyone and realize that these tools for smallpox, that is the vaccine, at least some way of giving it, existed long before WHO decided to have a program. But the people that were getting smallpox were the ones who were disenfranchised. They were the ones who were unemployed, in poverty, who had bias, that sort of thing. And so, it was very important to include the non-technical things. And in smallpox, I can tell you that every school and every church and every chief of a village and every volunteer that became involved was part of the solution of this.
Now, on the other hand, I can’t quite give up on smallpox eradication, even now, 40 plus years later. And I keep thinking of ways we could have improved. Nowadays, I would train dogs to pick up the scent of smallpox, because sometimes you would have beggar communities, people actually at the railroad station covered with a cloth with smallpox, but nobody knew that, but a dog would’ve picked that up right away. I’ve even come to the conclusion, if we were well enough organized, we could get rid of smallpox without vaccine and without the technical tools, the bifurcated needle, the jet injector and so forth. You would simply get people who are sick with smallpox and you would isolate them immediately and then you would follow all of their contacts. And the first symptom in a contact would get isolated and so on. And if you were organized well enough, you could get rid of smallpox without vaccine. So the tools are very important, but they’re not the last word.
Céline Gounder: Well, and in fact, that’s the approach that was used for Ebola. And now we have a vaccine. But most of the Ebola control efforts during the West African epidemic were really about that, identifying and isolating.
Helene, are we overly reliant on biomedical tools? And if we are overly reliant, should we pave the way for greater use of non-biomedical tools?
Helene Gayle: Well, as we know, the social determinants of health contribute more to health status than access to healthcare itself. So access to healthcare, including all the biomedical advances is necessary but not sufficient. I think we have to continue to think about why do we have some of the gaps in health that we know already exists. We look at the COVID pandemic as an example, where we know that the populations that were at greatest risk outside of age are people who lived in houses that were overcrowded or who had jobs that put them at risk, low wage earners, et cetera. So I think we have to think about both things. And I think back to your earlier question that is about people’s trust and mistrust, part of the trust in people being willing to access some of our biomedical tools comes from feeling that the rest of their needs are also being taken care of.
So if we just think of populations as we’ve got these great tools and we are going to give you these tools when your greatest challenge is whether or not you’re going to be able to feed your children at night or whether or not you’re going to have a roof over your head, you’re not going to be as eager and the uptake of our biomedical tools will not be as great. So I just think it’s about combining both and making sure that we’re thinking about some of these root causes that will also be part of helping to enhance, focusing on those will also be part of enhancing people’s trust and belief in some of the other approaches, that biomedical approaches that we know also make a huge difference.
Céline Gounder: Public health is different from clinical medicine, in that it focuses on the public or the ‘we’ so to speak, while clinical medicine focuses on the ‘I’ or the patient. There seems to be very little appetite in this moment for thinking about the ‘we.’
Bill, is there anything wrong with that? And if so, how do we shift that perspective that thinking about ‘we’ and public health and beyond?
Bill Foege: People often say clinical medicine deals with the numerator, the people that come to clinics and hospitals for care, while public health deals with the denominator. That’s simplistic because the denominator includes the numerator. And so, public health really is concentrated on everybody, on the ‘we’ and how to get everybody together on this.
There are two things from history that always impressed me. Confucius was asked by a student once, “Could you tell us in one word how best to live?” And Confucius said, “Is not reciprocity that word.” And so, this is ‘we’ that everybody’s dealing with each other. And then Gandhi said, his idea of the golden rule was that he should not enjoy something not enjoyed by everyone, the ‘we.’
So we keep hearing this from the wise people of history to stop thinking about just ourselves. Gandhi also said, “We should seek interdependence with the same zeal that we seek self-reliance.” And then he added in a soft voice, “There is no alternative.” And this is true. There is no alternative. And we’ve just got to take that approach in school, that’s much of school is built around how to improve your self-reliance, how to develop, how get money in the future and so forth. And we have to figure out how to teach interdependence.
Céline Gounder: Helene, should we be moving from an ‘I’ to a ‘we’ framing? And if so, how do we do that?
Helene Gayle: I think we have to. I think we recognize, and when we have pandemics, it’s very obvious. You can’t just think about what’s happening to you as an individual without recognizing that if we don’t stem transmission for something like a COVID, all of us are at risk.
So I think this sense of reciprocity is critical as we think about it. And it’s more broadly in our society. We can’t think that crime happens in one part of the city and it won’t also impact our economy, the economy of the city overall and ultimately impact other neighborhoods. I think we continue to think that we can wall off problems when we have to realize how interconnected we are, whether it’s health, whether it’s our economies, whether it’s the issue of climate change. I think as a species, we’re at a point where the ‘I’ thinking is having huge impacts for all of us. And unless we start having that ‘we’ mindset, we really are not going to be able to tackle some of these difficult wicked problems.
Bill Foege: If I could add one thing that Will Durant once said, ‘We will never do things globally unless we fear an alien invasion.” And what we’ve come up with are surrogates for alien invasions. So we see nuclear weapons as threatening of all of us. So we think ‘we.’ But there are other things. Our synthetic biology might be another one of these. Climate change may be a third one. We have four or five things that could totally eliminate people and we should be thinking ‘we’ in order to solve those problems.
Céline Gounder: So I’m now going to shift gears a little bit and take some of the questions our audience has been sending in. The first comes from Paurvi Bhatt who asks, “As we try to deal with new pandemics and eliminate older ones, how can we balance attention spans, science and safety in a world where “failing fast” and disruption define how we think about innovation?”
Helene, do you want to take a stab at that one?
Helene Gayle: Well, I just think we have to stay the course and continue to find ways. And we started out talking about health communications. I think we need to get better at our communications and in keeping people engaged in issues, because we are living in this 24/7 news cycle and a new issue coming up all the time. I think we as health professionals have an obligation to make sure that we are keeping these issues that are front and center in people’s minds and continuing to share what progress is happening. I think when people recognize there’s progress and you’re not just telling the same old story, I think you can keep people engaged, but I think it’s on us to do a better job in that regard.
Céline Gounder: Bill?
Bill Foege: I tell students now, and it took me a long time to reach this conclusion, that whenever they’re faced with these big problems, to think of three things.
Number one, try to get the science right. We’ve talked about you can’t always do that and you have to apologize and go back, but try to get the science right.
Number two, add art to the science. Will Durant says, “The first scientist that we know by name was Imhotep in Egypt, who was a physician and an artist and designed the step pyramid.” Because he said, “Then you get creative common sense at its best.” It was Huxley that says science is simply common sense at its best. So you get creative common sense at its best.
And then I go back 700 years to Roger Bacon who did a report for the Pope. And he said, “One of the problems with science is it has no moral compass.” And so you have to develop scientists with a moral compass. And when you do this, now you have moral creative common sense at its best, and this is a great approach to wicked problems.
Céline Gounder: Is public health science with a moral compass?
Bill Foege: It’s supposed to be. And sometimes we see it drifting off, but in general, public health people have a social mind that they’re trying to do this with a moral compass, including everyone.
Céline Gounder: Our next question comes from Merina Pradhan. Can you touch upon how the message needs to be as simple and brief as possible? Dr. Fauci’s message was very on point from a public health point of view, but how many in the general population would be able to assimilate that? Helene?
Helene Gayle: I would just say we have to tailor the message to the audience. When I saw the background that Dr. Fauci was talking against, I think he was talking to an audience of people who could incorporate that message. I might be wrong, but I think regardless, the point is if you’re sitting and talking to a group of public health professionals, you have one message. If you’re talking to the general public, you have another.
And I think it is true that we sometimes get confused with our own language because there’s so many nuances to public health that we put out these messages, that by the time we’re done, it’s hard to know. Do you believe yes, or do you believe no? So I agree. I think we have to keep it simple, but I think we also have to keep it truthful. And sometimes that’s a real challenge with the nuances of public health messaging. But I think again, tailoring it to the different audiences and recognizing that hopefully you have more than one bite at the apple, if you will, to make it short and concise, but then have other opportunities where you can explain it in greater detail.
Céline Gounder: Bill, this question is for you, from Mark Rosenberg, one of the new epidemics is the public health crisis of gun violence, now the leading cause of death for children and teens in the United States. Are there lessons from the eradication of smallpox that could be applied to help solve this new epidemic?
Bill Foege: I think all of the lessons from smallpox, knowing the truth, having coalitions, making sure that you progressing in the right way, having respect for culture, all of these things do apply. But I would end that answer, with becoming better ancestors, we’re saying that the ultimate expression of love from any of us is to become a better ancestor. And we certainly can do better on gun violence. And don’t put up with the discussion that says this is due to mental health problems and this and that, when other countries don’t have the same problem and they have just as much mental health problems as we do, but they don’t have the guns available.
Céline Gounder: Helene, this is a question from Ayo Femi-Osinubi. “Bill mentions that we don’t know what is sustainable till we try. How would you approach sustainability for pandemic preparedness in the midst of trying to prioritize basic health service delivery?”
Helene Gayle: Well, I think that the two aren’t necessarily in opposition. I think we need to have basic health services and building on basic services, making sure that we are thinking about how are those services available and sustainable so that when we have crises, public health crises, those systems are there and functional in a way that allows us to ramp up for public health emergencies.
So I think those things are not in opposition. It’s what I was talking about earlier. I think we need a more clear and comprehensive public health system that doesn’t just get ramped up every time we have a crisis, that it’s there, that it’s stable, that we have the kind of workforce that we need, that we have the kind of tools that we need, and that those are in place and that we build upon those than the other services that are important for individual care.
So again, I go back to a lot of this is about how we build systems that can be sustained and that are flexible and nimble so that they can respond when we have these public health crises.
Céline Gounder: So one last question. I’m going to give this one to Bill from David Torres. “I teach my global health students about the history of smallpox eradication. Given the coercive nature of the final push to vaccinate some people for smallpox and today’s resistance to and mistrust of public health measures, including vaccination campaigns and masking for COVID, would the elimination of smallpox be conceivable today? And if so, how would it be accomplished?”
Bill Foege: It would be very difficult today because of HIV and not knowing about immune systems, but you could still do it. The question about coercion, we hear this often, and most of this comes from one paper by Dr. Greenough, where he has interviewed people who worked on smallpox who used coercion. They would break into huts at 2:00 in the morning with the police officer to do that. None of that was necessary.
And so particular people were so enthusiastic about smallpox eradication that they did this. But think about it for a moment. If you have a village with three people who have refused vaccination, if they get smallpox, everyone around them is already vaccinated. They’re the ones that suffer. You don’t have to go in and use coercion. And so, when I’ve talked to other people who worked in smallpox, they’re surprised that anyone used coercion. You don’t have to do that, and that’s part of respecting the culture, is that you find other ways to do this.
Céline Gounder: Well, I really want to thank both of you, Bill and Helene for joining us today and for answering all of my questions, the audience’s questions. Between the two of you, you have over a century’s worth of wisdom in public health, and I always love hearing what you both have to say about these issues.
I just want to remind the audience that a recording of the event will be posted online later today and that all registrants will be sent an email when the recording is available. Also, please check out the podcast, Epidemic. It’s available on Apple, Spotify, wherever you get your podcasts. Season two is the season on eradication of smallpox. And also check out the Nine Lessons at ninelessons.org. And thanks everyone for joining us today.
Helene Gayle: Thank you.
Bill Foege: Thank you.
Season 2 of the ‘Epidemic’ Podcast Is ‘Eradicating Smallpox’
The eight-episode audio series “Eradicating Smallpox” documents one of humanity’s greatest public health triumphs.
By the late 1960s and early 1970s, smallpox was gone from most parts of the world. But in South Asia, the virus continued to kill. Public health heroes had to conquer social stigma, local politics, and more to wipe out the 3,000-year-old virus, an achievement many scientists thought was impossible.
Host Céline Gounder traveled to India and Bangladesh and brought back never-before-heard stories, many from public health workers whose voices have been missing in the coverage of the history of smallpox eradication. Gounder brings decades of experience working on tuberculosis and HIV in Brazil and South Africa; Ebola during the outbreak in Guinea, West Africa; and covid-19 in New York City at the height of the pandemic.
Season 2 of “Epidemic” is a co-production of KFF Health News and Just Human Productions.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
1 year 10 months ago
Multimedia, Public Health, Epidemic, Video
Seafood essential for women’s health
NUMEROUS studies have shown the benefits of seafood for women's health, as this category of food offers a wide range of health benefits due to the high nutrient content.
NUMEROUS studies have shown the benefits of seafood for women's health, as this category of food offers a wide range of health benefits due to the high nutrient content.
There are several types of seafood that are particularly beneficial — including salmon, mussels, tuna, and sardines, which support heart and brain health, and in some cases, reproductive health too.
"Seafood also helps with weight management, bone health, and skin health," explained nutritionist and dietician Claudhia Ashley. "It's important to choose a variety of seafood to maximise these benefits."
Here are some ways Ashley says seafood is good for women's health:
Omega-3 fatty acids
Seafood, especially fatty fish like salmon, mackerel, and sardines, is an excellent source of omega-3 fatty acids. These essential fats have been linked to heart health, reducing inflammation, and supporting brain function.
Heart and brain health
Omega-3 fatty acids found in seafood can help lower triglycerides, reduce blood pressure, and lower the risk of heart disease. They can also improve the ratio of "good" HDL cholesterol to "bad" LDL cholesterol. Also, Omega-3s, particularly docosahexaenoic acid (DHA), are crucial for brain development and function. Consuming seafood can support cognitive health and may even help reduce the risk of neurodegenerative diseases.
Bone health and weight management
Seafood like salmon and sardines are high in vitamin D and calcium, which are essential for maintaining strong bones and preventing conditions like osteoporosis. Lean protein found in seafood can contribute to feelings of fullness, helping with weight management and satiety.
Eye and skin health
Seafood is a good source of nutrients like vitamin A and DHA that promote eye health and may reduce the risk of age-related macular degeneration (eye disease that can blur your central vision). Omega-3s and antioxidants found in seafood can help maintain healthy skin by reducing inflammation and supporting collagen production.
Pregnancy and foetal development
Seafood is rich in nutrients like DHA that are essential for foetal brain and eye development during pregnancy. However, pregnant women should choose low-mercury options and avoid high-mercury fish.
Reduced depression and hormone regulation
The omega-3 fatty acids in seafood have been associated with a reduced risk of depression and can help manage mood disorders. Seafood provides nutrients like iodine and selenium, which are important for thyroid function and hormone regulation.
Reduced risk of certain cancers
Regular consumption of seafood has been associated with a reduced risk of certain cancers, such as breast and colorectal cancers.
Here are the best seafood options for your health:
Salmon and sardines
Rich in omega-3 fatty acids, especially DHA, salmon supports heart and brain health. It's also a good source of vitamin D and protein. Sardines are packed with omega-3s, calcium, and vitamin D, making them beneficial for bone health and overall well-being.
Trout
Similar to salmon, trout is rich in omega-3s, protein, and vitamin D. It's a great option for heart health and bone strength.
Shrimp
Low in calories and high in protein, shrimp is a good source of iodine, which is essential for thyroid function.
Mussels and oysters
Mussels are rich in vitamin B12, iron, and zinc, which are important for energy metabolism and immune system health. Oysters are high in zinc, which supports immune function and skin health. They also provide B vitamins and omega-3s.
Crab
Crab is a good source of protein, vitamin B12, and selenium. It's also low in mercury and a suitable option for women who are pregnant or breastfeeding.
Tuna (light canned) and herring
Light canned tuna is lower in mercury than albacore tuna and provides protein, omega-3s, and vitamin D. Herring is also high in omega-3s and vitamin D, making it beneficial for heart health and bone strength.
1 year 10 months ago
Influenza vaccine prevents spread of influenza virus; it’s getting closer
Influenza is a contagious respiratory disease; all people six months of age and older should receive it.
Influenza viruses are constantly changing; for this reason, every year, the composition of influenza vaccines is reviewed in the United States and updated as necessary to match as best as possible with the viruses, which, according to research, will be the most circulating in the season that is starting.
A detail
Dr. Jhan Gonzalez, a pulmonologist, indicates that the suggestions regarding the annual vaccination against influenza have some modifications, such as, for example, a change in the vaccination recommendations for people with egg allergy.
The specialist explains that the timing of influenza vaccination has not been modified; September and October are the best months for most people to get vaccinated. Vaccination is not recommended in July and August in most cases, but there are some considerations for certain groups of people in July and August.
Over 65 and pregnant women
For adults (especially those 65 years and older) and pregnant women in their first or second trimester, vaccination should be avoided in July and August unless they are not likely to be vaccinated in September or October.
Pregnant women in their third trimester can be vaccinated in July or August to ensure that their babies are protected against influenza at birth.
Children
Children who need two doses of influenza vaccine should receive their first dose as soon as it becomes available. The second dose should be given at least four weeks after the first dose. Vaccination in July or August may be considered for children who have medical appointments in these months if there will not be another opportunity. The physician from Centros de Diagnóstico y Medicina Avanzada y Telemedicina (CEDIMAT) assures that vaccination is still recommended as long as there is circulation of influenza viruses that pose a risk. In some seasons, this period may extend until the end of May or June. Gonzalez points out that the effectiveness of the influenza vaccine may depend in part on the coincidence between the vaccine’s viruses and those circulating.
Estimates
According to preliminary estimates, last season, people vaccinated against this disease had between 40% and 70% less risk of hospitalization due to influenza or its associated complications.
People with egg allergy
The significant change in influenza vaccination recommendations for 2023-2024 relates to administering the vaccine to egg-allergic persons. The physician says most current vaccines are still produced with an egg protein culture process and, therefore, contain a small amount of egg proteins, such as ovalbumin.
Recommendation
The CDC advises that the best way to reduce your risk of seasonal influenza and its potentially serious complications is to get vaccinated every year, this October.
1 year 10 months ago
Health, Local
Patience and love are required
TERRIFYING screams of "Help!" echoed throughout a community in St Thomas, late Monday night.
TERRIFYING screams of "Help!" echoed throughout a community in St Thomas, late Monday night.
Frightened by the calls, members of the community went to investigate. Upon arrival to the house where thecalls came from the people were informed that this was an elderly woman stuck in mental limbo. In her mind it was 1970, the year fire razed her house, almost killing her and her children.
This was the latest episode in her suffering from Alzheimer's disease. Embarrassment painted the face of her daughter as she held back tears, explaining, "She is ill. She thinks we are trying to keep her in a burning building," the woman, who requested anonymity, said.
The distraught woman added: "Last week she seh wi a try kill her and dem must call the ambulance. My mother was on top of her voice late at night shouting this. I had to let my neighbours know that she is suffering from dementia, just to not cause more alarm."
Similar stories are experienced worldwide by caregivers of individuals with dementia-related diseases, and the effects they have on those suffering weigh heavily on these persons who care for them as they too come to grips with shifting realities.
This World Alzheimer's Month the Jamaica Observer brings to the fore the issues caregivers, who are often overlooked, face. Come September 21, World Alzheimer's Day will be observed under the theme 'Never too early, never too late', with the aim being to identify risk factors and risk-reduction measures to prevent the onset of dementia.
Alzheimer's disease is defined by Johns Hopkin's Medicine as a progressive, neurodegenerative disease that occurs when nerves in the brain die. It destroys brain cells and nerves, disrupting the transmitters which carry messages in the brain, particularly those responsible for storing memories. According to Alzheimer's Disease International, it is the most common cause of dementia and accounts for 50-75 per cent of all cases.
The family caregivers play a critical role in the day-to-day care and protection of patients, even to their own detriment. How do they fare when dementia disrupts the flow of their and their loved ones' lives? Do they have enough support?
Alzheimer's Jamaica founder Dundeen Ferguson related her experience with Your Health Your Wealth.
"It was by virtue of my mother's diagnosis that Alzheimer's Jamaica was created," she stated.
"Caring for someone with Alzheimer's, in some respects there are challenges with money but otherwise she was really quiet and, you know, we would occasionally give her activities."
Studies have shown that apart from memory loss, other symptoms of Alzheimer's disease include difficulty performing familiar tasks; disorientation regarding time and place; poor or decreased judgement; changes in mood or behaviours, among others.
Fortunately for Ferguson her mother's behaviours were mild, but she was quick to point out that there are cases of "aggressive patients" who may cause harm to themselves and others. She encouraged other caregivers to expect a lot of unusual as well as unpredictable behaviours from loved ones, due to the illness.
"We just have to be careful and watch them so they don't harm themselves. My mom did things like pouring liquid detergent into a cup to drink because it looked like a juice, so we had to be vigilant in our care.
"It can be a toll sometimes, but patience and love are required. We have to understand that what they are doing is because of the disease."
Against that backdrop Ferguson said more needs to be done locally to spread awareness of the disease as well as provide support for patients and family, especially from a governmental level.
She added: "My mother was in Canada, where she was diagnosed. She lived there so she had the health-care system take care [and provide support to us]. So at the point where we could no longer manage at home, because everybody works and had to be out, we found a caregiver to sit with her during the days, and then later we had to put her in a nursing home."
In 2006, spurred by the first-hand experience she had with her mother, Ferguson founded Alzheimer's Jamaica to provide support to local patients and their caregivers as they navigate the challenges of Alzheimer's.
"It is a charitable organisation with the mission to provide support services for persons living with disease and dementia, dementia-related disorders. Families and caregivers are included in that group as well," she told Your Health Your Wealth.
Located in Kingston, Alzheimer's Jamaica became a member of Alzheimer's Disease International (ADI) — a not-for-profit international federation of Alzheimer's and dementia associations from around the world — since 2009. The local organisation hosted ADI's Caribbean Regional Conference in Kingston in 2019.
It also runs a Friends of Dementia Club, with some of the services provided by the association including educational events, resources (fact sheets, reading materials), seminars/webinars/workshops, and support groups.
Apart from support for the patient with the disease, "support groups and counselling services are available for family caregivers where they are advised of what to expect and how to handle the challenges presented with disease...so that they are better informed and know how to handle situations as they arise", Ferguson further emphasised.
She highlighted that many times caregivers are overwhelmed and need information with which to arm themselves so as to create a balance between caring for their loved ones as well as maintaining a healthy life. It can be taxing at times because caregivers sometimes have to forego their social activities, take leave from their jobs, in addition to the financial burden that comes with treatment/care for patients. The increasing stress of caregiving may adversely affect the physical and mental health of the caregivers.
"Your own personal mental health becomes important for you to take care of your loved ones as well... There were one or two times a month [when] a family member of mine went into a bit of depression — and that can happen — and we just knew how to deal with it.
"We meet regularly with caregivers to offer support and for them to share their experience and receive help. We also offer resources on external care such as nursing homes, etc."
She shared that help and resources are also available at The National Council of Senior Citizens. Moreover, the ADI collaborated with the World Health Organization (WHO) to produce the Help for Caregivers booklet, which ADI and the WHO distribute to better equip caregivers.
"We want to raise awareness of the disease and what our support services would include, so that's pretty much what we do — go to communities to raise awareness as it relates to Alzheimer's disease so that they are better informed on how [they] can handle their loved ones..."
She shared that often emphasis is placed on persons living with the disease but family members caring for patients also need support, and their well-being is just as important.
While everyone does not have the same experience, Dundeen explained that caregivers must be mindful of the disease's influence on their loved one's behaviour as they can sometimes be affected mildly while at other times the result can be aggressive behaviour.
1 year 10 months ago
'I Love My Life'
Bellevue Hospital on Wednesday, September 13 welcomed students from high schools in the Corporate Area for the first staging of its 'I love My Life' workshop.
Held in observance of World Suicide Prevention Month, the workshop was geared at equipping the students with knowledge to speak openly about mental health, identify signs of common mental illnesses, and access mental health resources.
The session featured presentations by Senator Dr Saphire Longmore, who is a psychiatrist; Dr Carolyn Jackson, executive clinical director of Caribbean Tots 2 Teens; and Dr Renee Rowe, medical officer at Bellevue Hospital.
In her presentation, Longmore shared strategies for teens to celebrate themselves and genuinely appreciate the hope that comes with being alive, despite obstacles and setbacks that teens often face.
Jackson delved into the mental health spectrum, and shared types of stress and different types of coping skills that teens use, and ways to develop resilience.
Rowe's presentation guided students gently into openly discussing the topic of suicide. In addition to sharing common contributing factors to suicide ideation and how students can manage them, Rowe also shared resources that students can utilise in times of need.
In welcoming the students to the event, Bellevue Hospital board member Khadrea Folkes urged each student to help break the stigma around mental health in their classes, schools, families and communities.
"One of the most powerful steps we can take is to break the silence and let our friends know that it's okay to talk about mental health; in fact, it's essential," she said.
"By speaking openly about our emotions, challenges, and experiences, we shatter the stigma that surrounds mental health issues. Through these conversations, we build a supportive community that empowers us and our friends to seek help when needed."
The students then had an opportunity to visit the hospital's public recreational space — Oo Park — where they enjoyed a painting session while sipping on cold beverages from the Milo truck that was on location.
Camille Campbell, public relations manager for the Anglo-Dutch Caribbean at Nestle, expressed that the manufacturing conglomerate is happy to renew its relationship with Bellevue Hospital, as it augers well for the development of mental health care in Jamaica, which is critical for overall health.
"The 'I Love My Life' workshop aligns seamlessly with MILO's mission to inspire and support the next generation. Together with Bellevue Hospital, we aim to foster a community of confident, resilient teenagers who are equipped to face life's challenges head-on. At Nestlé, we believe that a healthy body is the foundation for a happy life. We were excited to support this initiative that empowers young individuals to make positive choices for their well-being, nourishing their potential with the goodness of MILO."
1 year 10 months ago
Wisynco Group takes employee wellness to next level
WISYNCO Group Limited, a leading manufacturer and distributor in St Catherine, Jamaica, has taken bold steps to engender increased awareness of health, safety and well-being among its employees.
The entity recently opened the doors of a spacious, state-of-the-art fitness centre on the grounds of its head office in Lakes Pen, St Catherine. The facility, which currently offers standard gym equipment, group exercise sessions and on-site gym instructor to all employees, is open on weekdays from 6:00 am to 10:00 pm, and on Saturdays from 9:00 am to 4:00 pm.
The opening of the gym was one of the major highlights of the company's second staging of its Health, Safety and Well-being Month, which is geared towards educating and engaging employees on matters such as safety at work, safety on the road, and wellness initiatives that boost health and safety.
In 2022, August was declared Health, Safety and Well-being Month against the backdrop of the COVID-19 pandemic (which challenged the resilience and mental health of people worldwide) and a desire to continue safety education among employees at Wisynco.
During the month a number of activities are executed by a multidisciplinary team led by the human resources (HR) and health, safety and environment (HSE) departments.
According to Group Head of Human Resources Kisha-Ann Brown, the activities this year included financial wellness sessions, a Flash Fitness Invasion, Drift Dancing Challenge, Biggest Loser Weight Loss Challenge, the launch of Sagicor Day, numerous safety challenges, and visits of the Guardian Group Mobile Medical Unit to the company's Lakes Pen, White Marl, and Trelawny offices.
"These activities were geared towards empowering, engaging and educating employees about wellness in every sense of the word. At Wisynco we hold dear the holistic well-being and safety of all our employees. As a people-centred organisation whose mantra is to 'Improve the lives of our people', we know all too well that a healthier and safer workforce always equates to greater productivity and employee satisfaction."
The company culminated its month of activities on August 30th with its annual Health, Safety and Well-being Fair, which catered to more than 900 staff members.
Hundreds of staff members from various departments and locations turned up at the Lakes Pen Corporate Office to take advantage of the host of free medical examinations, safety demonstrations, and presentations that were available.
The health fair provided useful information about safety in manufacturing, safety in warehousing, safety in the offices and safety on the road.
Entities at the fair included Jamaica Cancer Society, Sagicor Group, Road Safety Unit, National Health Fund, Insight Optical, and National Council on Drug Abuse.
There was also a nurse's station that conducted free medical tests, three virtual reality tents, two snack bars, a games and activity tent, and an ambulance on standby.
By all indications, the staging of the Health, Safety and Well-being Fair was a huge success and the organisers are elated that the month of activities was well received by employees.
According to CEO Andrew Mahfood, the promotion of health and safety has always been top of the agenda at Wisynco.
He says, "In addition to our annual Health, Safety & Well-being Month initiatives, we are always working to spread awareness and participation in healthy lifestyle practices. We have a football field and netball/basketball court that have been keeping our employees active on a weekly basis, and with the gym opening we expect an even healthier population. Being the true innovators that we are we will continue to invest in our Wisynco family through education, infrastructure and engagement — thus further fostering the well-being of our staff in mind, body and soul."
1 year 10 months ago
Health Archives - Barbados Today
Back to School: Nutritious snacks on a budget
The Barbados Childhood Obesity Prevention Coalition (B-COP Coalition) continues its drive to prioritising children’s health. This time, it has donated 120 healthy hampers, filled with nutritious snacks for a week.
The recent implementation of the national school nutrition policy by the Ministry of Education, Technological and Vocational Training in April has sparked national attention and debate regarding access to affordable healthy food. B-COP Coalition, a leading advocate for this policy, has partnered with key sponsors to ensure these hampers are available, recognising that the back-to-school period can be both busy and costly for parents and guardians.
Dr Kia Lewis, the outgoing Chairperson of the B-COP Coalition, said: “In light of the new National School Nutrition Policy, the Coalition is very happy to roll out this Healthy Hamper: Back to School Edition, which is both healthy and cost-effective. We are targeting children in our childrens’ homes, at-risk youth, and our children in the Yute Gym of the Heart & Stroke Foundation.”
Dr Lewis further explained the initiative’s purpose, saying: “With this drive we wanted to show parents that it is possible to eat healthy on a budget. We know our schools have at least three water days, so the hampers have at least three bottles of water, an even cheaper way would be to buy a water bottle, you will also see several fruits in the hampers, given schools will be having two fruit days. Also, we have packed snacks as well, these are very reasonably priced and they would be compliant to the Alternative Snack and Beverage list, which shows the list of products on the market, which can be bought and given to our children for school.
“We are excited to launch this initiative and hope it assists Barbadian parents in making healthy choices for their children during school hours.”
This marks the B-COP Coalition’s second hamper drive, with the first taking place in 2020 during the COVID-19 Pandemic, targeting Barbadians with Non-Communicable Diseases (NCDs) who were more susceptible to the virus.
Several partners and sponsors made this initiative possible, including Signia Globe, Supreme Distributors, Guardian General, and the Church of the Latter Day Saints in Rendevous, where the hamper packing took place.
Marketing Officer of Signia Globe Richelle Lucas, commented: “We got a request and it was absolutely a no brainer for us to join with the Coalition. We know people think it is expensive to eat healthily, so we want to thank the Coalition for using these excellent examples of fruit and water. We are not saying that there are no snacks, yes there is a snack in the hampers but moderation is the key. Additionally, being able to work with the Heart and Stroke Foundation and get our children active and getting them active from young, so it sticks with them is important.” We are very happy to partner along with the Coalition and the other sponsors who have jumped on board for this worthy cause.
Meanwhile, Rhiyad Juman of Supreme Distributors said his firm was happy to give back to the community “by providing our 100 per cent natural Juices, our Fan juices and our Crystal Waters in order to provide for those children who may not know about the healthy options in Barbados. We are happy to help those who need the help” .
Expressing gratitude to the sponsors and partners for the initiative, Dr Lewis said: “We encourage corporate Barbados and other service groups to join us in supporting less fortunate children and fellow Barbadians as we collectively work towards a healthier way of life,’ she said. (PR)
The post Back to School: Nutritious snacks on a budget appeared first on Barbados Today.
1 year 10 months ago
A Slider, Business, Education, Health, Local News
Health Archives - Barbados Today
Man Aware gives youth vital info on sex and health
By Anesta Henry
Style met substance on Friday, as young males and the young at heart descended on the corner of Villa Road and Warner’s Road, Brittons Hill, for a fresh haircut and a healthy perspective on life.
Amid the celebration of style and camaraderie, there was a poignant reminder of the ongoing prevalence of HIV/AIDS in society.
Minister of People Empowerment and Elder Affairs Kirk Humphrey, took centre stage at the annual “Man Aware (Free Haircuts)” event. With his own close-cropped coiffure setting the tone, made an impassioned appeal to citizens to embrace safe sexual practices as a way of life. As he stood at a popular community junction, his message echoed: “HIV is still very real. It is still very prevalent.”
The event attracted children to get a fresh trim for back to school. But beyond the cool haircuts, it was a chance to interact with professionals who shared age-appropriate information about HIV/AIDS. It was a unique opportunity for the younger generation to learn about responsible living in a fun and engaging way.
While the Ministry of Health and Wellness is yet to reveal the latest statistics on Barbados’ HIV/AIDS prevalence, Humphrey said the Ministry of People Empowerment was playing its role as it relates to educating Barbadians about the importance of engaging in healthy sexual practices.
He said: “The numbers we have are from 2020. But I do think that regardless of the numbers, the truth is that it is clear to me that we have to be able to engage in sexual practices that are healthy.
“I think that a lot of people think that HIV is no longer there, and a lot of people are behaving as if HIV is no longer real. In many cases, because of the medication that you now have, it has gone from being a life-depriving illness to almost a chronic illness; it is still very prevalent.”
Encouraging Barbadians to get tested to know their HIV/AIDS status, Humphrey suggested that a person who knows they have a clean bill of health would refrain from engaging in unhealthy sexual practices.
People who have tested positive for HIV/AIDS would be aware that they must make the move to access medication, he added.
The Man Aware event went beyond haircuts by offering health check-ups, including blood pressure and sugar level assessments, in partnership with the Livewell Clinic. Humphrey highlighted the significance of these tests, emphasising that early detection can prevent life-altering non-communicable diseases.
“We are also working with the Livewell Clinic to be able to do health checks so that people can get their blood pressure checks and their sugar level checks to see if they are pre-diabetic or diabetic. This health check is one of the things that I think is going to be very important for the ministry.
“I think it is very important because a number of Barbadians are dealing with non-communicable issues, some of them becoming life-depriving in circumstances where they could be avoided if we get early testing and if we continue to do the things we are supposed to do, like eat right and make healthy choices. So, I want to thank the HIV/AIDS Commission for this work. I want to thank them for their constant advocacy, but I also feel like the time has come for Barbadians to recognise that the health choices we make in terms of what we eat also have consequences.”
The “Man Aware (Free Haircuts)” event, a blend of fashion and substance, continues to make its mark – one stylish haircut at a time – on Saturday at the Child Care Board, Cheapside, The City.
The post Man Aware gives youth vital info on sex and health appeared first on Barbados Today.
1 year 10 months ago
A Slider, Features, Health, lifestyle, Living Well, Local News