Mammograms at 40? Breast Cancer Screening Guidelines Spark Fresh Debate
While physicians mostly applauded a government-appointed panel’s recommendation that women get routine mammography screening for breast cancer starting at age 40, down from 50, not everyone approves.
Some doctors and researchers who are invested in a more individualized approach to finding troublesome tumors are skeptical, raising questions about the data and the reasoning behind the U.S. Preventive Services Task Force’s about-face from its 2016 guidelines.
“The evidence isn’t compelling to start everyone at 40,” said Jeffrey Tice, a professor of medicine at the University of California-San Francisco.
Tice is part of the WISDOM study research team, which aims, in the words of breast cancer surgeon and team leader Laura Esserman, “to test smarter, not test more.” She launched the ongoing study in 2016 with the goal of tailoring screening to a woman’s risk and putting an end to the debate over when to get mammograms.
Advocates of a personalized approach stress the costs of universal screening at 40 — not in dollars, but rather in false-positive results, unnecessary biopsies, overtreatment, and anxiety.
The guidelines come from the federal Department of Health and Human Services’ U.S. Preventive Services Task Force, an independent panel of 16 volunteer medical experts who are charged with helping guide doctors, health insurers, and policymakers. In 2009 and again in 2016, the group put forward the current advisory, which raised the age to start routine mammography from 40 to 50 and urged women from 50 to 74 to get mammograms every two years. Women from 40 to 49 who “place a higher value on the potential benefit than the potential harms” might also seek screening, the task force said.
Now the task force has issued a draft of an update to its guidelines, recommending the screening for all women beginning at age 40.
“This new recommendation will help save lives and prevent more women from dying due to breast cancer,” said Carol Mangione, a professor of medicine and public health at UCLA, who chaired the panel.
But the evidence isn’t clear-cut. Karla Kerlikowske, a professor at UCSF who has been researching mammography since the 1990s, said she didn’t see a difference in the data that would warrant the change. The only way she could explain the new guidelines, she said, was a change in the panel.
“It’s different task force members,” she said. “They interpreted the benefits and harms differently.”
Mangione, however, cited two data points as crucial drivers of the new recommendations: rising breast cancer incidence in younger women and models showing the number of lives screening might save, especially among Black women.
There is no direct evidence that screening women in their 40s will save lives, she said. The number of women who died of breast cancer declined steadily from 1992 to 2020, due in part to earlier detection and better treatment.
But the predictive models the task force built, based on various assumptions rather than actual data, found that expanding mammography to women in their 40s might avert an additional 1.3 deaths per 1,000 in that cohort, Mangione said. Most critically, she said, a new model including only Black women showed 1.8 per 1,000 could be saved.
A 2% annual increase in the number of 40- to 49-year-olds diagnosed with breast cancer in the U.S. from 2016 through 2019 alerted the task force to a concerning trend, she said.
Mangione called that a “really sizable jump.” But Kerlikowske called it “pretty small,” and Tice called it “very modest” — conflicting perceptions that underscore just how much art is involved in the science of preventive health guidelines.
Task force members are appointed by HHS’ Agency for Healthcare Research and Quality and serve four-year terms. The new draft guidelines are open for public comment until June 5. After incorporating feedback, the task force plans to publish its final recommendation in JAMA, the Journal of the American Medical Association.
Nearly 300,000 women will be diagnosed with breast cancer in the U.S. this year, and it will kill more than 43,000, according to National Cancer Institute projections. Expanding screening to include younger women is seen by many as an obvious way to detect cancer earlier and save lives.
But critics of the new guidelines argue there are real trade-offs.
“Why not start at birth?” Steven Woloshin, a professor at the Dartmouth Institute for Health Policy and Clinical Practice, asked rhetorically. “Why not every day?”
“If there were no downsides, that might be reasonable,” he said. “The problem is false positives, which are very scary. The other problem is overdiagnosis.” Some breast tumors are harmless, and the treatment can be worse than the disease, he said.
Tice agreed that overtreatment is an underappreciated problem.
“These cancers would never cause symptoms,” he said, referring to certain kinds of tumors. “Some just regress, shrink, and go away, are just so slow-growing that a woman dies of something else before it causes problems.”
Screening tends to find slow-growing cancers that are less likely to cause symptoms, he said. Conversely, women sometimes discover fast-growing lethal cancers soon after they’ve had clean mammograms.
“Our strong feeling is that one size does not fit all, and that it needs to be personalized,” Tice said.
WISDOM, which stands for “Women Informed to Screen Depending On Measures of risk,” assesses participants’ risk at 40 by reviewing family history and sequencing nine genes. The idea is to start regular mammography immediately for high-risk women while waiting for those at lower risk.
Black women are more likely to get screening mammograms than white women. Yet they are 40% more likely to die of breast cancer and are more likely to be diagnosed with deadly cancers at younger ages.
The task force expects Black women to benefit most from earlier screening, Mangione said.
It’s unclear why Black women are more likely to get the most lethal breast cancers, but research points to disparities in cancer management.
“Black women don’t get follow-up from mammograms as rapidly or appropriate treatment as quickly,” Tice said. “That’s what really drives the discrepancies in mortality.”
Debate also continues on screening for women 75 to 79 years old. The task force chose not to call for routine screening in the older age group because one observational study showed no benefit, Mangione said. But the panel issued an urgent call for research about whether women 75 and older should receive routine mammography.
Modeling suggests screening older women could avert 2.5 deaths per 1,000 women in that age group, more than those saved by expanding screening to younger women, Kerlikowske noted.
“We always say women over 75 should decide together with their clinicians whether to have mammograms based on their preferences, their values, their health history, and their family history,” Mangione said.
Tice, Kerlikowske, and Woloshin argue the same holds true for women in their 40s.
This article was produced by KFF Health News, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
2 years 2 months ago
Aging, california, Race and Health, States, Cancer, HHS, Preventive Services, Preventive Services Task Force, Women's Health
PAHO/WHO | Pan American Health Organization
Countries agree to prioritize initiatives to improve the health of Indigenous populations
Countries agree to prioritize initiatives to improve the health of Indigenous populations
Cristina Mitchell
29 May 2023
Countries agree to prioritize initiatives to improve the health of Indigenous populations
Cristina Mitchell
29 May 2023
2 years 2 months ago
PAHO/WHO | Pan American Health Organization
Novel products, misleading information threaten to undo decades of gains against tobacco use
Novel products, misleading information threaten to undo decades of gains against tobacco use
Cristina Mitchell
29 May 2023
Novel products, misleading information threaten to undo decades of gains against tobacco use
Cristina Mitchell
29 May 2023
2 years 2 months ago
Medical News, Health News Latest, Medical News Today - Medical Dialogues |
Vitamin D deficiency adversely impacts neuronal growth and dopamine function in brain
Australia: A recent study published in the Journal of Neurochemistry has shown how vitamin D deficiency impacts neurons' development, contributing to disorders such as schizophrenia.
Australia: A recent study published in the Journal of Neurochemistry has shown how vitamin D deficiency impacts neurons' development, contributing to disorders such as schizophrenia.
Using innovative technology, neuroscientists discovered that a lack of vitamin D changes neuron growth and affects the brain's dopamine release mechanism. They found that in the cells grown in the presence of vitamin D, dopamine release was enhanced.
"Our findings show the importance of vitamin D in the structural differentiation of dopaminergic neurons and suggest that maternal vitamin D deficiency might alter how early dopaminergic circuits form," Darryl Eyles, University of Queensland, Saint Lucia, Queensland, Australia, and colleagues wrote in their study.
Previous studies have shown vitamin D to be a critical factor in dopaminergic neurogenesis and differentiation. Also, developmental vitamin D (DVD) deficiency has been associated with disorders of abnormal dopamine signalling with a neurodevelopmental basis, such as schizophrenia. Schizophrenia is linked with several developmental risk factors, both environmental and genetic. There is no precise information on the neurological causes of the disorder, but it is known that schizophrenia is associated with a change in how the brain uses dopamine.
In the present study, the researchers provided further evidence of the role of vitamin D as a mediator of dopaminergic development by showing that it increases neurite outgrowth, presynaptic protein re-distribution, neurite branching, dopamine production and functional release in various in vitro models of developing dopaminergic cells including primary mesencephalic cultures, SH-SY5Y cells, and mesencephalic/striatal explant co-cultures.
The research team at the Queensland Brain Institute developed dopamine-like cells to replicate the differentiation process into early dopaminergic neurons that usually occur during embryonic development.
They cultured the neurons in the absence and presence of the active vitamin D hormone. They then showed alterations in the distribution of presynaptic proteins responsible for dopamine release within these neurites. In three different model systems, dopamine neurite outgrowth was markedly increased.
Using false fluorescent neurotransmitters, a new visualization tool, the team analyzed the functional changes in presynaptic dopamine uptake and release in the absence and presence of vitamin D. They found that in the cells grown in the presence of the hormone, the dopamine release was enhanced compared to a control.
Key takeaways from the study:
- For the first time, the study has shown that chronic exposure to the active vitamin D hormone increases the capacity of developing neurons to release dopamine and continues to establish vitamin D as an essential differentiation agent for developing dopamine neurons.
- This study also has implications for understanding the mechanisms behind the link between DVD deficiency and schizophrenia.
- Dopamine release was enhanced in cells grown in the presence of the vitamin D hormone compared to a control.
The research team believes that such early alterations to dopamine neuron differentiation and function may be the neurodevelopmental origin of dopamine dysfunction later in adults with schizophrenia.
Reference:
Nedel Pertile, R. A., Brigden, R., Raman, V., Cui, X., Du, Z., & Eyles, D. Vitamin D: A potent regulator of dopaminergic neuron differentiation and function. Journal of Neurochemistry. https://doi.org/10.1111/jnc.15829
2 years 2 months ago
Medicine,Neurology and Neurosurgery,Medicine News,Neurology & Neurosurgery News,Top Medical News
Outpatient clinic relocated to General Hospital building Phase 2
Effective Tuesday, 30 May 2023, outpatient clinics will be conducted at the new hospital building (Phase 2)
View the full post Outpatient clinic relocated to General Hospital building Phase 2 on NOW Grenada.
Effective Tuesday, 30 May 2023, outpatient clinics will be conducted at the new hospital building (Phase 2)
View the full post Outpatient clinic relocated to General Hospital building Phase 2 on NOW Grenada.
2 years 2 months ago
Health, PRESS RELEASE, general hospital, gis, Ministry of Health, outpatient clinic
Stop smoking...before it stops you! - Trinidad & Tobago Express Newspapers
- Stop smoking...before it stops you! Trinidad & Tobago Express Newspapers
- Breaking the Addiction: Strategies to Help You Quit Smoking News18
- How to make quitting smoking, tobacco use possible India Today
2 years 2 months ago
Stop smoking...before it stops you! - Trinidad & Tobago Express Newspapers
- Stop smoking...before it stops you! Trinidad & Tobago Express Newspapers
- Are you a smoker? Dr. Deepak Khanna alarms on the health risks you might be putting yourself into. midday india
- How to make quitting smoking, tobacco use possible India Today
- Here’s how to quit smoking this No Tobacco Day | Why is smoking so addictive? Doctor answers midday india
- View Full Coverage on Google News
2 years 2 months ago
Medical News, Health News Latest, Medical News Today - Medical Dialogues |
Oral dexamethasone effective in treatment of infantile spasms and related Lennox-Gastaut syndrome
Oral dexamethasone is effective in the treatment of infantile spasms and infantile spasms related Lennox-Gastaut syndrome suggests a new study published in the BMC Pediatrics
Treatment with adrenocorticotropic hormone (ACTH) or a corticosteroid is the first choice for infantile spasms (IS), and vigabatrin is the first choice for children with tuberous sclerosis. Although corticosteroids may be also effective against IS and IS-related Lennox–Gastaut syndrome (LGS), the use of dexamethasone (DEX), a kind of corticosteroid, for these diseases has been rarely reported. This retrospective study aimed to evaluate the efficacy and tolerability of DEX for the treatment of IS and IS-related LGS.
Patients diagnosed as having IS (including patients whose condition evolved to LGS after the failure of early treatment) in our hospital between May 2009 and June 2019 were treated with dexamethasone after failure of prednisone treatment. The oral dose of DEX was 0.15–0.3 mg/kg/d. Thereafter, the clinical efficacy, electroencephalogram (EEG) findings, and adverse effects were observed every 4–12 weeks depending on the individual patient’s response. Then, the efficacy and safety of DEX in the treatment of IS and IS-related LGS were retrospectively evaluated.
Results
Among 51 patients (35 cases of IS; 16 cases of IS-related LGS), 35 cases (68.63%) were identified as responders to DEX treatment, comprising 20 cases (39.22%) and 15 cases (29.41%) with complete control and obvious control, respectively. To discuss the syndromes individually, complete control and obvious control were achieved in 14/35 and 9/35 IS cases and in 6/16 and 6/16 IS-related LGS cases, respectively. During DEX withdrawal, 11 of the 20 patients with complete control relapsed (9/14 IS; 2/6 LGS). The duration of dexamethasone treatment (including weaning) in most of the 35 responders was less than 1 year. However, 5 patients were treated with prolonged, low-dose maintenance therapy, which continued for more than 1.5 years. These 5 patients showed complete control, and 3 patients had no recurrence. Except for one child who died of recurrent asthma and epileptic status 3 months after stopping DEX, there were no serious or life-threatening adverse effects during DEX treatment.
Oral DEX is effective and tolerable for IS and IS-related LGS. all LGS patients were evolved from IS in this study. The conclusion may not apply to patients with other etiology and courses of LGS. Even when prednisone or ACTH is failed, DEX may still be considered as a treatment option. For children who respond to DEX but do not show complete control after 6 months of treatment, prolonged treatment with low-dose DEX administered in the morning might be considered.
Reference:
Li, J., Gao, Y., Cao, J. et al. Efficacy analysis of oral dexamethasone in the treatment of infantile spasms and infantile spasms related Lennox–Gastaut syndrome. BMC Pediatr 23, 255 (2023). https://doi.org/10.1186/s12887-023-04062-6
2 years 2 months ago
Pediatrics and Neonatology,Pediatrics and Neonatology News,Top Medical News
The high price of back pain
BACK pain is a common and often debilitating condition that affects millions of people worldwide. Besides the physical discomfort and limitations it imposes on individuals, back pain also comes with significant financial costs. In this article we explore the economic impact of back pain and highlight the importance of selecting an effective management strategy, particularly through the utilisation of physiotherapy.
The economic burden of back pain
Back pain is a leading cause of disability and absenteeism in the workplace, resulting in substantial financial losses for both individuals and society as a whole. The costs associated with back pain can be categorised into direct health-care expenses, indirect costs due to lost productivity, and intangible costs related to reduced quality of life.
1. Direct Health Care Expenses
Back pain patients often seek medical intervention including doctor visits, diagnostic tests, medications, and surgical procedures. These expenses can quickly accumulate, especially for chronic or severe cases. According to a study published in The Journal of the American Medical Association (JAMA), the annual cost of treating back pain in the United States alone exceeds US$100 billion.
2. Indirect Costs and Lost Productivity
Back pain frequently leads to missed workdays, decreased work productivity, and limitations in job performance. The Global Burden of Disease Study estimated that in 2017 low back pain alone accounted for 60.1 million years lived with disability globally. This translates into an enormous economic burden encompassing productivity, increased sick leave, and disability benefits.
3. Intangible Costs
Beyond the measurable financial expenses, back pain also has intangible costs such as reduced quality of life, psychological distress, and decreased overall well-being. The impact on mental health, relationships, and social activities can further contribute to the overall burden experienced by individuals suffering from chronic back pain.
THE ROLE OF PHYSIOTHERAPY IN MANAGING BACK PAIN
Physiotherapy, a specialised branch of health care, offers a conservative, non-invasive approach to managing back pain. It focuses on assessing and treating musculoskeletal conditions, including back pain, through a variety of evidence-based techniques. Physiotherapists are highly trained professionals who utilise manual therapy, exercise prescription, education, and other modalities to improve mobility, reduce pain, and enhance functional ability.
Targeted Treatment
Physiotherapy employs personalised treatment plans tailored to the individual's specific needs. Through a thorough assessment, physiotherapists identify the underlying causes of back pain such as muscle imbalances, joint dysfunction, or poor posture. By addressing these root causes physiotherapy aims to alleviate pain and improve overall function.
Active Rehabilitation
Unlike passive treatment methods such as medications or surgeries, physiotherapy emphasises active rehabilitation. Patients are actively involved in their own recovery process, learning exercises, stretches, and strategies to manage and prevent future episodes of back pain. This empowers individuals to take control of their health, reducing the risk of recurrent pain.
Holistic Approach
Physiotherapy takes a holistic approach to back pain management, considering the whole body and its interconnected systems. This comprehensive perspective allows physiotherapists to address not only the symptoms but also the contributing factors that may exacerbate or perpetuate back pain. By improving overall physical fitness, posture, and body mechanics, physiotherapy promotes long-term pain relief and better spinal health.
The economic burden of back pain is staggering, affecting individuals, employers, and society at large. Choosing an effective management strategy is crucial to mitigate the financial costs associated with back pain. Physiotherapy offers a valuable solution by providing targeted treatment, active rehabilitation, and a holistic approach to back pain management. To access exceptional physiotherapy services that prioritise your back care and alleviate the cost of back pain, consider seeking help from InSync Health Wellness Beauty. With their team of highly trained physiotherapists and commitment to patient-centred, one-on-one care, InSync Health Wellness Beauty is a premier choice for addressing your back pain concerns and improving your overall well-being.
Kimberly Hoffman is a pelvic health therapist and director of InSync Health Wellness Beauty. Follow her on
Instagram:
be.insync or contact her by calling or sending a
WhatsApp
message to 876-804-3665
2 years 2 months ago
'Fuel your health, not tobacco use'
JAMAICA joins the rest of the world in celebrating World No Tobacco Day 2023 with the theme 'Fuel your health, not tobacco use', raising awareness about the dangers of tobacco and nicotine use.
This year's theme focuses on the need for comprehensive legislation to protect present and future generations from the dangers of tobacco and nicotine use, and the importance of leading a healthy lifestyle free from tobacco or vaping.
According to the 2017 Jamaica Health and Lifestyle Survey, 15 per cent of Jamaicans aged 15 years and older currently use tobacco products. In addition, a significant number of Jamaican students are using tobacco and electronic cigarettes. Currently, 11.2 per cent of students (11.1 per cent of boys and 10.9 per cent of girls) smoke cigarettes, while 11.7 per cent of students (13.7 per cent of boys and 9.7 per cent of girls) use electronic cigarettes.
The impact of tobacco use is a significant public health concern in Jamaica, with 50 per cent of lifetime smokers starting by the age of 19, and 10 per cent starting as young as age 11. Tobacco is attributable to 11 per cent of all noncommunicable diseases, six per cent of all cardiovascular diseases, and 71 per cent of deaths from cancer of the trachea, bronchus, and lung in Jamaica.
To address this problem, Jamaica has implemented a series of tobacco control measures aimed at reducing tobacco and nicotine use among the population. These measures include a ban on smoking in public places, increased taxes on tobacco products, and the introduction of graphic health warnings on cigarette packaging. Recent achievements in tobacco control measures in Jamaica include the process of implementing the Tobacco Control Act (2020) which was tabled in Parliament in December 2020.
As we celebrate World No Tobacco Day 2023 it is essential to highlight the importance of leading a healthy lifestyle that is free from tobacco smoke and vape clouds. We encourage all Jamaicans to take personal responsibility for their health by quitting smoking or vaping, and adopting a healthy lifestyle.
We also urge the Government to move quickly in implementing comprehensive legislation to protect people, especially youth, from the deadly effects of tobacco and nicotine. It is critical to invest in tobacco control programmes and services, raise public awareness, and enforce laws and regulations to reduce the prevalence of tobacco and nicotine use in Jamaica.
Let us work together to create a tobacco-free Jamaica where everyone can live a healthy and fulfilling life.
2 years 2 months ago
AHF Jamaica wants top priority for menstrual health
GLOBAL health-care organisation, AIDS Healthcare Foundation (AHF) Jamaica is urging the Jamaican Government to prioritise menstrual health as a comprehensive public health issue, as it seeks to increase awareness around period poverty and other related issues facing women.
According to Dr Kevin Harvey, Caribbean regional director for AHF and head of the School of Public Health and Health Technology at the University of Technology, Jamaica (UTech), "Menstrual health is a public health and human rights issue that, if addressed in a holistic manner, can enable the progress of sustainable development in Jamaica and improve the well-being of our women, girls, and the men who support them."
Dr Harvey's comments come ahead of today's World Menstrual Hygiene Day celebration, a global effort aimed at, among other things, ending period poverty — a condition affecting millions of women and girls worldwide.
Period poverty refers to the limited access that many women have to menstrual hygiene products, menstrual education, and proper water sanitation and hygiene facilities.
In addressing these menstrual health challenges AHF Jamaica has donated over 100,000 sanitary hygiene products to women and girls in need across the island. However, the organisation acknowledges that product distribution alone is insufficient as a multilateral issue like menstrual health requires institutional and structural intervention, research, and consistent efforts to bridge the gap between social and structural determinants and their impact on women and girls.
"To complicate matters," says Harvey, "the socio-economic impacts of external shocks such as the ongoing COVID-19 pandemic have worsened menstrual health challenges, especially for lower-income families and female-headed households which often have to choose between buying food or menstrual hygiene products."
AHF Jamaica has therefore targeted menstrual health as a holistic public health matter, addressing limited access to period products, menstrual education, adequate sanitation and water facilities, and combating stigma and cultural norms.
The organisation has also emphasised the importance of training health-care workers in menstrual disorders and gender-responsive approaches to understanding the needs and requirements of those affected.
With Jamaica currently in the season of constitutional reform, AHF Jamaica sees an opportunity to engage in discussions about menstrual leave as a tool of empowerment for positive changes in women's menstrual health.
The organisation remains dedicated to advocating for menstrual health and achieving menstrual equity. By prioritising a holistic approach and addressing the multifaceted challenges associated with menstrual health, AHF Jamaica believes that period poverty and other related menstrual hygiene challenges can be eradicated by 2030.
2 years 2 months ago
9 alternative health-care financing models for Jamaican informal sector operators
IN low-resource nations like Jamaica, there are several health-care financing models that could mitigate the various limitations of traditional health insurance and could be potentially beneficial for patients, especially the very large pool of patients in the informal economic sectors. These options aim to increase access to health-care services and reduce financial barriers. When considering health-care coverage for people employed in the informal sector in developing countries, a financial model that suits their unique needs and circumstances is crucial. Last week, we explored the concept of alternative health-care financing models for informal sector workers in Jamaica who are traditionally excluded from traditional health insurance schemes. In our column today, we will explore some of these specific models in more detail.
1. National health insurance. Implementing a national health insurance system can provide coverage for the entire population. This approach pools resources from various funding sources, such as taxes, premiums, or contributions, to finance health-care services. It ensures that essential health services are available to everyone, regardless of their current health status, age or ability to pay. This is often referred to as Universal Health Insurance and is widely available to citizens of many countries where health care is recognised as a national imperative. The social contract between the state and the citizens as well as the nexus between good health care and economic development form the bedrock of the advocacy for universal health insurance.
2. Community-based health financing. This approach involves establishing community-based health insurance schemes or micro-health insurance programmes. These programmes are designed to meet the needs of specific communities or low-income groups and can be tailored to the needs of informal sector workers, considering their irregular incomes and specific health-care needs. They often involve contributions from members of the community, which are used to cover health-care costs. Community health financing can be effective in reducing the burden of health-care expenses on individuals. For this to work, there must be a sense of community that obligates people to sign on to such schemes even when they may not be immediate beneficiaries. Many communal living societies in Asia and Africa embrace this concept because of cultural socialisation. By organising at the community level, these models can promote solidarity, local ownership, and accountability. Examples of successful community-based health insurance schemes include the Mutuelles in Rwanda and the Community Health Fund in Tanzania.
3. Social health protection programmes. These programmes target vulnerable populations, such as the poor, informal sector workers, and marginalised groups. They provide financial risk protection by offering subsidies or exemptions for health-care services. Social health protection programs can be funded through government allocations, donor support, or a combination of both. They may offer exemptions, subsidies, or reduced-cost services to ensure affordable health-care access. Ghana's National Health Insurance Scheme and Thailand's Universal Coverage Scheme are examples of successful social health protection programmes.
4. Health savings accounts. Health savings accounts allow individuals to set aside funds specifically for health-care expenses. These accounts are usually paired with high-deductible insurance plans, where individuals pay out-of-pocket costs up to a certain threshold. Health savings accounts can empower individuals to make informed decisions about their health care spending and provide a safety net for unexpected medical expenses. In some countries, tax incentives are provided to individuals to encourage health savings accounts. In such situations, funds contributed to a health savings account is exempt from taxes up to a specified limit. However, penalties and taxes would accrue if such funds are used for anything other than health care.
5. Donor funding and grants. Low-resource nations can seek support from international organisations, NGOs, and philanthropic foundations to secure funding for health-care services. Donor funding and grants can be used to improve infrastructure, strengthen health-care systems, and provide subsidies or grants to individuals who cannot afford essential health care. HIC Foundation has used grants to support individuals seeking certain services at HIC, for example. Our current HIC Save a Life programme is based on generous grant support from HIC Foundation allowing qualified patients with heart attack and unstable cardiac conditions to obtain angiogram, angioplasty with stent and hospital admissions at about 30 per cent of the usual costs with the rest paid for by HIC Foundation grant.
6. Public-private partnerships. Collaborations between the public and private sectors can help leverage resources and expertise to improve health-care financing. Public-private partnerships can involve contracting private health-care providers to deliver services, establishing insurance programmes with private sector participation, or engaging in joint initiatives to address specific health-care challenges.
7. Microinsurance. Microinsurance refers to insurance products designed for low-income individuals or households, including those in the informal sector. These products typically have low premiums and simplified administrative processes. Microinsurance plans can provide coverage for specific health-care services or a package of essential health benefits. They can be offered through partnerships between insurance providers, microfinance institutions, and community-based organisations. Examples include the Health Insurance Fund in India and the Kilimo Salama (Safe Agriculture) initiative in Kenya.
8. Government subsidies and vouchers. Governments can provide targeted subsidies or vouchers to informal sector workers to help cover health-care costs. These subsidies can be used to purchase health insurance, health-care subscriptions or access specific services at reduced costs. By directly supporting individuals in the informal sector, governments can increase their access to health care without creating an additional administrative burden for them. The Seguro Popular programme in Mexico and the Rashtriya Swasthya Bima Yojana (RSBY) in India have employed this approach. This is an approach that can be effective in Jamaica especially if targeted at informal sectors that have brought prosperity and global recognition for Jamaica like the creative industries, specifically musicians and music producers and sports, notably track and field athletes.
9. Mobile-based health financing. Leveraging mobile technology can be an effective approach to reach and engage informal sector workers. Mobile-based health financing models can include mobile payment platforms, mobile savings accounts, or mobile insurance applications. These models facilitate easy premium payments, claims processing, and access to healthcare services. Examples include M-TIBA in Kenya and Aavaz Health in India.
It's important to note that the suitability and effectiveness of these health-care financing options may vary depending on the specific context and needs of each community. Additionally, partnerships between governments, private sector entities, and community-based organisations are often crucial for the success of these initiatives. The suitability of these financial models depends on the specific context, resources, and infrastructure available in each developing country. It is important to consider the preferences, needs, and capacities of the informal sector workers themselves, involving them in the design and implementation of the financial model.
Implementing a combination of approaches tailored to the local circumstances is often necessary to achieve sustainable, inclusive and equitable health-care financing.
Dr Ernest Madu, MD, FACC and Dr Paul Edwards, MD, FACC are consultant cardiologists for the Heart Institute of the Caribbean (HIC) and HIC Heart Hospital. HIC is the regional centre of excellence for cardiovascular care in the English-speaking Caribbean and has pioneered a transformation in the way cardiovascular care is delivered in the region. HIC Heart Hospital is registered by the Ministry of Health and Wellness and is the only heart hospital in Jamaica. Send correspondence to
info@caribbeanheart.com
or call 876-906-2107.
2 years 2 months ago
Vector Control Department intensifies mosquito fogging
The Vector Control Department will intensify its ongoing fogging operations over the week of 23–28 May 2023
View the full post Vector Control Department intensifies mosquito fogging on NOW Grenada.
The Vector Control Department will intensify its ongoing fogging operations over the week of 23–28 May 2023
View the full post Vector Control Department intensifies mosquito fogging on NOW Grenada.
2 years 2 months ago
Health, Notice, PRESS RELEASE, dengue, fogging, gis, Ministry of Health, mosquito destruction act, vector control department
“Miracle drugs” swarm on social networks in the Dominican Republic, Public Health wants to control it
Santo Domingo.- The sale of uncertified medicines through social media platforms without any medical endorsement is a growing concern for health authorities in the Dominican Republic.
Santo Domingo.- The sale of uncertified medicines through social media platforms without any medical endorsement is a growing concern for health authorities in the Dominican Republic. Minister of Public Health, Daniel Rivera, raised the alarm about these “miracle drugs” being promoted without scientific backing, often using influencers or false advertising to attract buyers.
Many of these products are being advertised on social networks, claiming numerous benefits and even employing popular figures and influencers to entice consumers. People often fall victim to scams when purchasing these products. Rivera stressed the need for increased controls and intervention to address this issue, while also urging the public to remain vigilant and ensure that the products they buy or consume have proper regulation and certification.
Rivera cited an example from last year when his own image was used without consent to endorse blood pressure products, a situation he promptly denounced. The responsibility of verifying the regulation and certification of medicines, as well as suspending and removing counterfeit or expired products, falls under the General Directorate of Medicines, Food, and Health Products of the Ministry of Public Health (Digemaps).
The Minister encouraged the public to ensure that health products and services they consume or purchase have the proper regulation, certification, or authorization issued by the Ministry of Public Health to guarantee their quality. He further revealed that 137 centers have been shut down this year for non-compliance with licensing regulations.
The Dominican Republic recently hosted the “Congress of Central American Drug Regulatory Agencies,” where 12 Latin American nations aimed to strengthen controls in the marketing of consumer products. The participating countries, including Costa Rica, El Salvador, Guatemala, Honduras, Nicaragua, and Panama, sought to establish common regulations and controls at the regional level. The Pan American Health Organization (PAHO) reiterated its commitment to providing technical cooperation requested by member states to strengthen drug regulatory authorities in Central America and the Dominican Republic.
2 years 2 months ago
Health
Children with asthma ‘bounce back’ with symptom control, lung function after COVID-19
WASHINGTON — Children with asthma did not see any significant differences in lung function or symptom control up to 18 months after acute COVID-19, according to data presented at the American Thoracic Society International Conference.These results indicate that COVID-19 does not impact long-term severity or control among children with asthma, Kristina M.
Gaietto, MD, MPH, clinical instructor of pediatrics and postdoctoral scholar, division of pediatrics, University of Pittsburgh School of Medicine and UPMC Children’s Hospital of Pittsburgh, and colleagues wrote.“Obviously,
2 years 2 months ago
World Anti-Doping Agency gives ultimatum to the Dominican Republic
Santo Domingo.- On August 4th, the Dominican Republic will be celebrating the 20th anniversary of the 2003 Pan American Games held in its capital city.
Santo Domingo.- On August 4th, the Dominican Republic will be celebrating the 20th anniversary of the 2003 Pan American Games held in its capital city. However, if the Ministry of Sports and Recreation (Miderec) fails to address the repeated warnings from the World Anti-Doping Agency (WADA), the country could face severe international sanctions, including restrictions on its athletes’ participation in global events as a neutral team without their flag and anthem.
The situation parallels the challenges faced by Russian athletes following a 2019 sanction for violating the World Anti-Doping Code. In a communication/ultimatum sent by María José Pesce, the director of WADA’s Latin American office, to Miderec and the Dominican Olympic Committee (COD) on May 4th, it was stated that unless 15 suggested corrective actions are taken by August 4th, the non-compliance chapter of the World Anti-Doping Code will be activated, leading to significant consequences for Dominican athletes and the country as a whole.
The core issue revolves around the lack of financial allocation to the National Anti-Doping Agency, with an estimated annual funding of no more than RD$10 million. Failure to comply with the World Anti-Doping Code can result in the withdrawal of all financial and logistical assistance from WADA. Additionally, the suspension of recognition by the Olympic and Paralympic Movements could be imposed, preventing the country from organizing official competitions and participating in specific events.
The alert from WADA comes at a crucial time as the Dominican Republic prepares to participate in the upcoming Central American and Caribbean Games in El Salvador and faces potential disqualification from major events such as the Pan American Games in Santiago, Chile, and the qualifying competitions for the 2024 Paris Olympic Games.
To avoid such consequences, WADA’s letter emphasizes the need for financial resources to meet the requirements of the World Anti-Doping Code. This includes addressing the recommendations outlined in the audit conducted in the country in December, implementing a control distribution plan, conducting a risk analysis, complying with technical analysis documents, and establishing an adverse results management unit.
The urgency of the matter necessitates action from Miderec and the COD to ensure compliance and secure the future participation of Dominican athletes in international sporting events.
2 years 2 months ago
Health, Sports
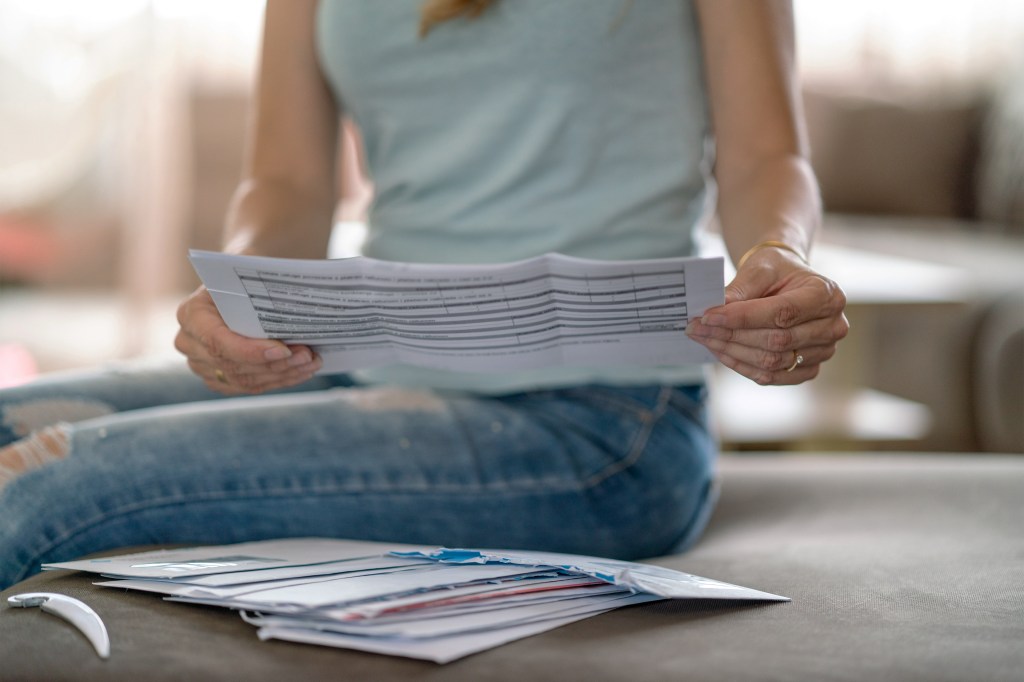
Denials of Health Insurance Claims Are Rising — And Getting Weirder
Millions of Americans in the past few years have run into this experience: filing a health care insurance claim that once might have been paid immediately but instead is just as quickly denied.
If the experience and the insurer’s explanation often seem arbitrary and absurd, that might be because companies appear increasingly likely to employ computer algorithms or people with little relevant experience to issue rapid-fire denials of claims — sometimes bundles at a time — without reviewing the patient’s medical chart. A job title at one company was “denial nurse.”
It’s a handy way for insurers to keep revenue high — and just the sort of thing that provisions of the Affordable Care Act were meant to prevent. Because the law prohibited insurers from deploying previously profit-protecting measures such as refusing to cover patients with preexisting conditions, the authors worried that insurers would compensate by increasing the number of denials.
And so, the law tasked the Department of Health and Human Services with monitoring denials both by health plans on the Obamacare marketplace and those offered through employers and insurers. It hasn’t fulfilled that assignment. Thus, denials have become another predictable, miserable part of the patient experience, with countless Americans unjustly being forced to pay out-of-pocket or, faced with that prospect, forgoing needed medical help.
A recent KFF study of ACA plans found that even when patients received care from in-network physicians — doctors and hospitals approved by these same insurers — the companies in 2021 nonetheless denied, on average, 17% of claims. One insurer denied 49% of claims in 2021; another’s turndowns hit an astonishing 80% in 2020. Despite the potentially dire impact that denials have on patients’ health or finances, data shows that people appeal only once in every 500 cases.
Sometimes, the insurers’ denials defy not just medical standards of care but also plain old human logic. Here is a sampling collected for the KFF Health News-NPR “Bill of the Month” joint project.
- Dean Peterson of Los Angeles said he was “shocked” when payment was denied for a heart procedure to treat an arrhythmia, which had caused him to faint with a heart rate of 300 beats per minute. After all, he had the insurer’s preapproval for the expensive ($143,206) intervention. More confusing still, the denial letter said the claim had been rejected because he had “asked for coverage for injections into nerves in your spine” (he hadn’t) that were “not medically needed.” Months later, after dozens of calls and a patient advocate’s assistance, the situation is still not resolved.
- An insurer’s letter was sent directly to a newborn child denying coverage for his fourth day in a neonatal intensive care unit. “You are drinking from a bottle,” the denial notification said, and “you are breathing on your own.” If only the baby could read.
- Deirdre O’Reilly’s college-age son, suffering a life-threatening anaphylactic allergic reaction, was saved by epinephrine shots and steroids administered intravenously in a hospital emergency room. His mother, utterly relieved by that news, was less pleased to be informed by the family’s insurer that the treatment was “not medically necessary.”
As it happens, O’Reilly is an intensive-care physician at the University of Vermont. “The worst part was not the money we owed,” she said of the $4,792 bill. “The worst part was that the denial letters made no sense — mostly pages of gobbledygook.” She has filed two appeals, so far without success.
Some denials are, of course, well considered, and some insurers deny only 2% of claims, the KFF study found. But the increase in denials, and the often strange rationales offered, might be explained, in part, by a ProPublica investigation of Cigna — an insurance giant, with 170 million customers worldwide.
ProPublica’s investigation, published in March, found that an automated system, called PXDX, allowed Cigna medical reviewers to sign off on 50 charts in 10 seconds, presumably without examining the patients’ records.
Decades ago, insurers’ reviews were reserved for a tiny fraction of expensive treatments to make sure providers were not ordering with an eye on profit instead of patient needs.
These reviews — and the denials — have now trickled down to the most mundane medical interventions and needs, including things such as asthma inhalers or the heart medicine that a patient has been on for months or years. What’s approved or denied can be based on an insurer’s shifting contracts with drug and device manufacturers rather than optimal patient treatment.
Automation makes reviews cheap and easy. A 2020 study estimated that the automated processing of claims saves U.S. insurers more than $11 billion annually.
But challenging a denial can take hours of patients’ and doctors’ time. Many people don’t have the knowledge or stamina to take on the task, unless the bill is especially large or the treatment obviously lifesaving. And the process for larger claims is often fabulously complicated.
The Affordable Care Act clearly stated that HHS “shall” collect the data on denials from private health insurers and group health plans and is supposed to make that information publicly available. (Who would choose a plan that denied half of patients’ claims?) The data is also supposed to be available to state insurance commissioners, who share with HHS the duties of oversight and trying to curb abuse.
To date, such information-gathering has been haphazard and limited to a small subset of plans, and the data isn’t audited to ensure it is complete, according to Karen Pollitz, a senior fellow at KFF and one of the authors of the KFF study. Federal oversight and enforcement based on the data are, therefore, more or less nonexistent.
HHS did not respond to requests for comment for this article.
The government has the power and duty to end the fire hose of reckless denials harming patients financially and medically. Thirteen years after the passage of the ACA, perhaps it is time for the mandated investigation and enforcement to begin.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
2 years 2 months ago
Health Industry, Insurance, Health IT, HHS
PAHO/WHO | Pan American Health Organization
Lanzan Alianza Mundial de Oxígeno para impulsar el acceso al oxígeno médico que salva vidas
Global Oxygen Alliance launched to boost access to life saving oxygen
Cristina Mitchell
25 May 2023
Global Oxygen Alliance launched to boost access to life saving oxygen
Cristina Mitchell
25 May 2023
2 years 2 months ago
ECCB’s 40th Anniversary Lecture Series Grenada Edition 31 May
The Grenada Edition of the ECCB’s 40th Anniversary Lecture Series starts at 7 pm on Wednesday, 31 May 2023, at the Radisson Grenada Beach Resort
View the full post ECCB’s 40th Anniversary Lecture Series Grenada Edition 31 May on NOW Grenada.
The Grenada Edition of the ECCB’s 40th Anniversary Lecture Series starts at 7 pm on Wednesday, 31 May 2023, at the Radisson Grenada Beach Resort
View the full post ECCB’s 40th Anniversary Lecture Series Grenada Edition 31 May on NOW Grenada.
2 years 2 months ago
Business, Health, PRESS RELEASE, Travel/Tourism, angus friday, eastern caribbean central bank, eccb, grenada citizenship by investment, medical tourism, richard duncan
Temporary Relocation of Chief Pharmacist and Pharmacy Inspector’s Office
The office of the Chief Pharmacist and Pharmacy Inspector has been temporarily relocated to the ground floor of the new wing (phase 2) of the General Hospital, St George’s
View the full post Temporary Relocation of Chief Pharmacist and Pharmacy Inspector’s Office on NOW Grenada.
The office of the Chief Pharmacist and Pharmacy Inspector has been temporarily relocated to the ground floor of the new wing (phase 2) of the General Hospital, St George’s
View the full post Temporary Relocation of Chief Pharmacist and Pharmacy Inspector’s Office on NOW Grenada.
2 years 2 months ago
Business, Health, Notice, PRESS RELEASE, chief pharmacist, general hospital, gis, Ministry of Health, pharmacy inspector