Control blood pressure, control cardiovascular disease
THE global rise in the prevalence and mortality of cardiovascular diseases (CVD) over the past 30 years is thought to indicate the real world outcomes of the profound income inequality and health inequity within communities resulting from the unmet need for affordable interventions.
This inequity is compounded by patients' risk factor level, education and health policies.
In a recent report evaluating data from 204 countries and territories in the Global Burden of Cardiovascular Disease Collaboration, the investigators identified Central Asia and Eastern Europe as epicentres of the CVD epidemic with the highest rates of CVD mortality. Furthermore, the report identified hypertension, dietary indiscretion, high cholesterol, and air pollution as the leading causes of CVD globally. The recognition of air pollution as a leading cause of CVD globally is an area that has received scant attention. Starting from the new year, we intend to do a series of articles on air pollution and CVD to highlight this important but neglected cause of CVD.
In high-income regions of North America the researchers found that age-standardised CVD mortality rates ranged from 102.1 to 224.8 per 100,000 in 2021, reflecting a 2.6-fold difference. Hypertensive heart disease had the largest per cent increase in CVD cause-specific, age-standardised mortality rates since 1990 (53.3 per cent), whereas rheumatic heart disease had the largest per cent decrease (61.2 per cent).
Ranking of modifiable risk factors
The analysis of the Global Burden of Diseases, Injuries and Risk Factors study provide a useful ranking of modifiable risk factors associated with these trends in CVD and mortality:
• High systolic BP
•Dietary risks
• High LDL-Cholesterol
• Air pollution
• High body mass index (BMI)
• Tobacco smoking
• High blood glucose
• Kidney dysfunction.
According to the analysis, rheumatic heart disease, fuelled by poverty and crowded housing conditions, as well as alcoholic cardiomyopathy fuelled by excessive alcohol consumption, are also potential targets for CV risk reduction.
Global prevalence of CVD and mortality
Globally, the total number for CVD nearly doubled over the past 30 years from 271 million in 1990 to 523 million in 2019, and CVD deaths increased from 12.1 million in 1990 to 18.5 million in 2019, affecting men and women almost equally (9.6 million men: 8.9 million women), according to the analysis. Approximately 6.1 million premature deaths from CVD were noted in individuals aged 30 to 70 years, representing 33 per cent of CVD deaths worldwide. Additionally, CVD was the underlying cause of death among approximately one-third of all deaths globally. CVD prevalence is likely to increase substantially as a result of population growth and ageing, especially in low-resource communities including much of Africa, Asia, Latin America, and the Caribbean where the share of older persons is projected to double between 2019 and 2050. Increased attention to promoting ideal cardiovascular health and healthy ageing across the lifespan and population segments must therefore form part of the national policy thrust for managing the expected increase in CVD in the coming years. We look forward to working with the Government and other responsible parties in proactively designing mechanisms to address this problem in a way that ensures health equity consistent with the One Health initiative being promoted by the Minister of Health Dr Christopher Tufton.
Disability-Adjusted Life Years (DALY)
The report also looked at disability-adjusted life years, the years of life lost due to premature mortality, and years lived with disability. By summing the DALYs in a population, we can discover which populations are living with the greatest health burden and prioritise those areas for future health interventions. The main advantage is that DALYs provide a composite, internally consistent measure of population health which can be used to evaluate the relative burden of different diseases and injuries, and provide comparison of population health by geographic region and over time. The overall burden of disease is assessed using the disability-adjusted life year (DALY), a time-based measure that combines years of life lost due to premature mortality (YLLs) and years of life lost due to time lived in states of less than full health, or years of healthy life lost due to disability (YLDs). DALY is a very useful assessment of quality of life rather than simply measuring the length of life. Next to ischemic heart disease and stroke, the collaborative investigators found that hypertensive heart disease had the highest age-standardised DALY rate of 226.4. Among all CVD risks, hypertension accounted for the largest proportion of DALYs at 40.5 per cent. Globally, the report noted that ischemic heart disease is the leading cause of CV death, accounting for 9.44 million deaths in 2021 and 185 million DALYs.
Hypertension is a leading modifiable risk for CVD
Hypertension is the leading modifiable risk factor for CV death. High blood pressure remains the key risk factor driving the global rise in CVD mainly through the causation of hypertensive heart disease, coronary artery disease and stroke. According to the Jamaica Health and Lifestyle Survey for 2016/2017, one in three Jamaicans are hypertensives, including nearly 40 per cent of women. More worrisome is that four out of every 10 hypertensives are unaware of their status, 60 per cent of whom are men. Another study from the Imperial College of London notes that more than 80 per cent of hypertensives globally account for about one billion people live in low- and middle-income countries.
In individuals at risk, treatment to lower blood pressure is a remarkably effective strategy to delay progression to cardiovascular complications including heart attacks, strokes, kidney failure and heart failure. When initiated in middle age, intensive blood pressure control is predicted to prolong life expectancy by up to three years. In light of the evidence, there is a great urgency in driving public health strategies to promote early screening, detection, and treatment of hypertension. Affordable and cost-effective approaches must be explored to expand access to include individuals in remote, rural, and low-income communities. Effective strategies currently exist leveraging mobile technology and remote patient monitoring to expand access, and these approaches must be embraced in low-resource nations and communities to address a clear and present danger. Individuals at risk can be evaluated in real time, and early signs of cardiovascular damage can be identified with simple techniques like electrocardiograms (ECGs). Affordable technology currently exists to provide electrocardiograms daily — with cardiologist interpretation in real time in all public health centres in all 14 parishes — and we would be happy to assist the Ministry of Health and Wellness in getting this done. Once identified, treatment approaches must consider the use of polypills for hypertension and other CVD promoters as these have been demonstrated to be highly cost-effective and efficacious, especially in individuals and communities with financial constraints.
Dr Ernest Madu, MD, FACC and Dr Paul Edwards, MD, FACC are consultant cardiologists for the Heart Institute of the Caribbean (HIC) and HIC Heart Hospital. HIC is the regional centre of excellence for cardiovascular care in the English-speaking Caribbean and has pioneered a transformation in the way cardiovascular care is delivered in the region. HIC Heart Hospital is registered by the Ministry of Health and Wellness and is the only heart hospital in Jamaica. Send correspondence to info@caribbeanheart.com or call 876-906-2107
2 years 7 months ago
2023 health goals
Happy
New Year! January 1 is a time when we sit and set resolutions, many of which we discard before the month ends. However, in life, goals are important and those goals should consist of health-based targets for living a more rewarding life in tip-top shape. Below are seven health goals we should set and work towards achieving this year.
Happy
New Year! January 1 is a time when we sit and set resolutions, many of which we discard before the month ends. However, in life, goals are important and those goals should consist of health-based targets for living a more rewarding life in tip-top shape. Below are seven health goals we should set and work towards achieving this year.
1. Walk more
Ten minutes a day of brisk walking can increase circulation, lift your spirits, and enhance sleep. If you want to increase your walking in 2023, try breaking it up into 10-minute sessions to make it less intimidating. Remember, if while walking you can talk but your breathing is faster than usual, you are walking briskly enough.
2. Spend less time sitting down
The body wasn't designed to sit in front of the TV or at a desk for long periods of time. It raises your chances of developing diabetes; cardiovascular disease; and breast, colon, and colorectal cancer. Why not break up your desk time with the Pomodoro method? Set a timer so that each hour will be divided into two 25-minute blocks and two 5-minute pauses. During the work periods concentrate on your work, and during the breaks move around. Make use of your breaks to stand up, perform a quarter squat, rotate, or simply take a lap around the office. When you're working, this strategy can improve your concentration.
3. Plan meals
Just purchasing what you need reduces calories and waste, while saving you money. Before you go shopping, take the time to plan your meals and make a list.
4. Make sure you're enrolled for 2023 health insurance coverage
Do you have health insurance next year? If you aren't sure, now's the time to double-check. Call your insurance providers and review your existing plans or make an appointment to get some amount of coverage. It's protection you need when you least expect it.
5. Schedule your annual check-ups
Most individuals don't enjoy going to the doctor, especially if everything seems to be in order. However, as the saying goes, "An ounce of prevention is worth a pound of cure." Plan a time for your yearly check-up or well-woman appointment. Remember to schedule a dental cleaning or two while you have your calendar out.
6. Drink more water
Drinking a few more glasses of water each day can significantly improve your general health, particularly in warm weather or when you are exercising hard. The daily recommended intake is eight glasses of water. A glass typically measures eight ounces so a simple way is to invest in a 64 ounce bottle, fill it with water and complete it by the end of the day. If you don't like plain water, flavour it with infused fruit, herbs, or tea bags, but avoid processed sugar, sodas, and other artificially sweetened beverages.
7. Improve your sleep hygiene
Good sleep hygiene is crucial for both physical and mental health. You likely already know some of the simplest advice for getting more rest: consistent pattern, avoid using screens at least 30 minutes before bedtime, and keep phones away and on mute. It's important to get those eight hours in.
2 years 7 months ago
Medical News, Health News Latest, Medical News Today - Medical Dialogues |
Increasing prevalence of sleep disorders may increase CVD burden in future
Iran: Sleep disorders are linked with several health problems, including depression, coronary artery disease, and anxiety. A study investigated the predictors, prevalence, and health impacts of hypersomnia and insomnia in southeastern Iran and the five-year incidence rate (IR) of these sleep disorders.
The study's results, published in the Iranian Journal of Psychiatry, showed high prevalence and increasing sleep disorder trends in the past five years. If not addressed, the community's cardiovascular disease (CVD) burden will significantly increase in the future due to sleep disorders and the associated risk factors.
Sleep disorders are conditions that lead to changes in the way of sleeping. A sleep disorder can affect safety, quality of life, and overall health. Not getting desired sleep can impact the ability to drive safely and raises the risk of other health problems. Some common sleep disorders are sleep apnea, insomnia, narcolepsy, and restless legs syndrome.
The study was a single-stage, cross-sectional, cluster sampling ((KERCADR study phase two) study that examined nine CAD risk factors, including sleep disorders. The study comprising 9997 participants, 15 to 80 years old, was carried out in Kerman. Abdolreza Sabahi, Kerman Universit of Medical Sciences, Kerman, Iran, and colleagues assessed medical examination along with demographic, sleep status, anxiety, depression status (Beck Inventories), and Physical activity level (GPAQ). A fasting blood sample was taken for lipid and blood glucose analysis. Out of 9997 included participants, 59.4% were females.
The authors reported the following findings:
- 45.3% of the participants suffered from hypersomnia and insomnia, which was 15% more than the phase 1 prevalence.
- Participants with insomnia had a higher chance of being anxious. Still, participants with hypersomnia had a higher chance of being depressed, being a cigarette smoker, an opium user, and being sedentary.
- Regarding marital status, the hypersomnia prevalence was as follows in increasing order of prevalence: singles > married > widowed > divorced.
- The incidence rate (IR) of insomnia was higher in females, and a higher IR of hypersomnia were seen in males.
- The incidence rate of both sleep disorders was more significant in people with Low Physical Activity (LPA).
"The findings showed a high current prevalence and increasing sleep disorders trend in the past five years," the authors wrote. "If not addressed properly, the CVDs burden in the community will show a significant increase in the future due to sleep disorders and other associated risk factors."
Reference:
Najafipour H, Sabahi A, khoramipour kayvan, Shojaei Shahrokhabad M, Banivaheb G, Shadkam M, Mirzazadeh A. Prevalence, Incidence and Health Impacts of Sleep Disorders on Coronary Artery Disease Risk Factors: Results of a Community-Based Cohort Study (KERCADRS). Iran J Psychiatry. 2022;17(3):247-256.
2 years 7 months ago
Cardiology-CTVS,Medicine,Psychiatry,Cardiology & CTVS News,Medicine News,Psychiatry News,Top Medical News
The Dominican Republic strives to contain the focus of cholera in the capital
A cholera prevention operation is making door-to-door visits in Santo Domingo’s La Zurza neighborhood when a man staggers out to meet them, visibly weakened after a week of showing symptoms of the disease, as he explains to the group.
Public Health personnel, accompanied by Pan American Health Organization (PAHO) members, direct him to one of the tents set up by the Ministry in this sector of the Dominican capital, on the banks of the Isabela River, where the majority of the country’s ten cases of the disease have been confirmed.
Romer Castro expends his last energy to reach the provisional care center, where they begin the standard protocol for a patient with the symptoms: diarrhea, vomiting, stomach pain, and dehydration picture. He has taken too long to arrive for treatment, according to the health personnel of the mobile hospital, who are used to foreign patients who are afraid to go to the doctor, especially if they have irregular immigration status.
After giving him first aid, they transport him to the Moscoso Puello Hospital, accompanied by a relative and one of the doctors in charge of the case, so that the necessary tests can be performed to confirm if it is cholera, as there are other conditions, such as parasitism, that present with similar symptoms.
2 years 7 months ago
Health, Local
Dominican Republic will have the cholera vaccine
After two new cases of cholera were reported in 13 people in La Zurza, the Pan American Health Organization (PAHO) reported that the Dominican Republic will have the vaccine that counteracts the spread of the disease as soon as possible.
At a press conference, the interim representative of the international organization in the country, Bernardino Vitoy, pointed out that they still do not have the arrival date of the vaccine, but that they are in the middle of the negotiations so that in the future the serum can be placed the vulnerable population.
“World production is not very high, there are few suppliers and an estimate is currently being made of how much it will be possible to allocate to the Dominican Republic,” he said. The doctor also stated that they are working to expand the diagnostic capacity of the pathology, with the delivery of more rapid tests so that infections can be confirmed and ruled out.
According to experts, the cholera vaccine is administered orally and two doses are placed so that it can have the necessary effects.
2 years 7 months ago
Health
Medical News, Health News Latest, Medical News Today - Medical Dialogues |
19 eminent doctors appointed to NMC, its various boards
New Delhi: 19 eminent doctors have been selected as part-time members of the medical advisory council of the National Medical Commission (NMC).
The Union Minister for Health and Family Welfare, Dr Mansukh Mandaviya took part in the appointment process through a draw of lots.
The procedure of appointments is laid down in National Medical Commission (NMC) Act, 2019.
New Delhi: 19 eminent doctors have been selected as part-time members of the medical advisory council of the National Medical Commission (NMC).
The Union Minister for Health and Family Welfare, Dr Mansukh Mandaviya took part in the appointment process through a draw of lots.
The procedure of appointments is laid down in National Medical Commission (NMC) Act, 2019.
All appointments comprised 10 Part-time Members from State/UT governments, 9 Part-time Members from State Medical Council, fourth Member of each Autonomous Board and One expert for Search Committee.
As per the NMC act 2019, these appointments are being done for two years. Members from various states/UTs have been selected in the following categories:
1. Ten Part-time Members of NMC are selected from the nominee of the State / UT Government in Medical Advisory Council (earlier appointed in 2020): Assam, Arunachal Pradesh, Chhattisgarh, Puducherry, Uttarakhand, Ladakh, Sikkim, Telangana, Karnataka and Kerala.
Smt. Krishna Gohain, retired IAS officer and a Vice Chancellor of Srimanta Sankaradeva University of Health Sciences has been nominated from Assam. He was earlier appointed as the Secretary to the Education Department, Govt. of Assam.
Prof. Saket Kushwaha, Vice Chancellor of Rajiv Gandhi University of Health Sciences from Arunachal Pradesh. He is an Indian agricultural scientist and economist and has published more than a dozen books and a look at them indicates the wide range of his scholarly aptitude. Prior to Rajiv Gandhi, he served as a vice-chancellor, department dean or professor-in-charge at several universities including Banaras Hindu University and Lalit Narayan Mithila University.
Prof. Dr. Gurmeet Singh, Vice Chancellor of Puducherry University selected from Puducherry. He is a renowned academic administrator and an internationally reputed expert in the field of corrosion science and smart materials. During 2011-2012, Prof. Singh served as a Chair Professor at Lunghwa University, Taipei, where he was specially invited to start collaborative research. He was a visiting scientist to Hungary and Japan and has been on academic assignments to Germany, Italy, Australia, Singapore, Korea, Thailand and Kenya.
Prof. Hem Chandra, Vice Chancellor of Hemwati Nandan Bahuguna Health University, Dehradun from Uttarakhand. Prof. (Dr.) Hem Chandra, before joining as Vice-Chancellor, HNB Uttarakhand Medical Education University, Dehradun, was Head of Department of Hospital Administration & Medical Superintendent, Sanjay Gandhi Postgraduate Institute of Medical Sciences (SGPGIMS) Lucknow, UP.
Prof. S. K. Mehta, Vice Chancellor of University of Ladakh. Dr Mehta is a fellow of the Royal Society of Chemistry and has served as the director of PU's Sophisticated Analytical Instrumentation Facility (SAIF). He has more than 360 publications in international journals of repute to his name, 8,400 citations and is an author of as many as 15 books/chapters. He has been nominated as a member of several national committees.
Lt. Gen. (Dr.) Rajan Singh Grewal, Vice Chancellor of Sikkim Manipal University. He superannuated as Director General Medical Services (Army) in 2020, after 38 years of distinguished meritorious service in various prestigious academic, professional, administrative leadership & staff appointments under Ministry of Defence. He was appointed as Honorary Surgeon to the President of India in 2019. He has received various prestigious honours & awards.
Dr. Karunakar Reddy, Vice Chancellor of Kaloji Naryana Rao University of Health Sciences from Telangana. He is a member of the Expert Committee on the COVID-19.
Dr Ashok Chandraker, Vice Chancellor of Pandit Deendayal Upadhyaya Memorial Health Science and Ayush University of Chhattisgarh.
Dr. M. K. Ramesh, Vice Chancellor of Rajiv Gandhi University of Health Sciences has been selected from Karnataka. He in the past has served the University as Registrar (Evaluation). Previously, Dr. S. Sacchidanand served as the VC of the institute and he retired on 14 June.
Dr. Mohanan Kunnummal, Vice Chancellor of Kerala University of Health and Sciences, Thrissur from Kerala. Dr. Mohanan was a professor at the Department of Radio Diagnosis at Thrissur Medical College for a long time. In 2016, he was appointed as the principal of Manjeri Government Medical College. After retirement, he was working as the head of the Department of Radio Diagnosis in Perinthalmanna MES Medical College.
2. Nine Part-time Members of NMC are selected from the nominee of State Medical Council in Medical Advisory Council (earlier appointed in 2020): Andhra Pradesh, Haryana, Goa, Gujarat, Delhi, Odisha, Himachal Pradesh, Punjab and Rajasthan
Dr. Mahesh Babulal Patel, Vice Chancellor of Gujarat University. He was a Professor of Pathology at B. J. Medical College in Ahmedabad (Gujarat).
Dr. Deepak Sharma from Rajasthan.
Dr. Vijay Kumar from Punjab.
Dr. Rajiv Sood, Founder and Dean of ABVIMS & Dr RML Hospital's Department of Urology & Renal Transplant from Delhi. A master specialist in the field of Urology, he was instrumental in the creation of the Department at RML Hospital and has been heading its Urological Services since its inception in 1996.
Dr. Vinod Kashyap, registrar at the Himachal Pradesh Medical council.
Prof. Datteswar Hota is an eminent Renal Transplant Surgeon at the S.C.B Medical College, Cuttack in Odisha. He is also the recipient of the BC Roy Lifetime achievement award.
Dr. Padmanabh Vaman Rataboli, who was the president of the Goa Medical Council, is among the five members, who have been reelected to the council.
Dr. R. K. Aneja, President of the Haryana Medical Council.
Dr. Buchipudi Sambasiva Reddy is the president of the Andhra Pradesh Medical Council.
3. Fourth Member of each Autonomous Board (part-time Member) from the nominee of State Medical Council in Medical Advisory Council (earlier appointed in 2020) have been selected.
Dr. Pallavi P. Saple, administrator of the Maharashtra Medical Council and has been nominated for Undergraduate Medical Education Board in Maharashtra. Dr Saple was a former student of JJ Hospitals itself. She also served as the professor and the head of the paediatric department in the institute. Dr Pallavi Saple became one of the youngest deans to take charge of the institute.
Dr. K Senthil has been selected for Post-Graduate Medical Education Board in Tamil Nadu. Dr K Senthil is an MD General Medicine and a Prof of Medicine in Madurai Medical College.He has been Practicing in a village in Madurai district - Checkanurani, since 1990 after completing his MD and serving the poor and rural people around the area for last 32 years. He has also been serving as the President of TN Medical Council for the last 7 years and Also been the State President of TN Govt Doctors Association for last 16 years continuously.
Dr. Urmila Singh has been selected for Medical Assessment and Rating Board from Uttar Pradesh.
Dr. Sahajanand Prasad Singh is a consultant general surgeon and National President of the Indian Medical Association (IMA). Dr Singh also served as the President of the Bihar Chapter of the Indian Medical Association. He has been nominated for Ethics and Medical Registration Board
4. One expert from Odisha was nominated for the Search Committee.
Prof. Datteswar Hota is an eminent Renal Transplant Surgeon at the S.C.B Medical College, Cuttack and has been nominated for the Search Committee from Odisha. He is also the recipient of the BC Roy Lifetime achievement award.
List of the names of experts can be found below. For maintaining transparency in the draw of lots, media personnel was also present to record the event.
Shri Rajesh Bhushan, Union Health Secretary, Dr. Manohar Agnani, Additional Secretary, Dr. Sachin Mittal, Joint Secretary along with officials from Health Ministry were present during the event.
Selected Members from States/ UTs
S No
Name of State/ UT
Name of the Member
1
Assam
Smt. Krishna Gohain, IAS (Retd.), Vice Chancellor, Srimanta Sankaradeva University of Health Sciences
2
Arunachal Pradesh
Prof. Saket Kushwaha Vice Chancellor Rajiv Gandhi University of Health Sciences
3
Puducherry
Prof. Dr. Gurmeet Singh, Vice Chancellor, Puducherry University
4
Uttarakhand
Prof. Hem Chandra , Vice Chancellor Hemwati Nandan Bahuguna Health University, Dehradun
5
Ladakh
Prof. S. K. Mehta, Vice Chancellor, University of Ladakh
6
Sikkim
Lt. Gen. (Dr.) Rajan Singh Grewal, Vice Chancellor, Sikkim Manipal University
7
Telangana
Dr. Karunakar Reddy, Vice Chancellor, Kaloji Naryana Rao University of Health Sciences
8
Chattisgarh
Dr Ashok Chandraker, Vice Chancellor, Pandit Deendayal Upadhyaya Memorial Health Science and Ayush University of Chhattisgarh
9
Karnataka
Dr. M. K. Ramesh, Vice Chancellor, Rajiv Gandhi University of Health Sciences
10
Kerala
Dr. Mohanan Kunnummal, Vice Chancellor, Kerala University of Health and Sciences, Thrissur, Kerala
Selected Members from Various State Medical Councils
S No
Name of State Medical Council
Name of the Member
1
Gujarat
Dr. Mahesh Babulal Patel
2
Rajasthan
Dr. Deepak Sharma
3
Punjab
Dr. Vijay Kumar
4
Delhi
Dr. Rajiv Sood
5
Himachal Pradesh
Dr. Vinod Kashyap
6
Odisha
Prof. Datteswar Hota
7
Goa
Dr. Padmanabh Vaman Rataboli
8
Haryana
Dr. R. K. Aneja
9
Andhra Pradesh
Dr. Buchipudi Sambasiva Reddy
Selected Members (Part-Time) for Autonomous Boards of NMC
S No
Name of State Medical Council
Name of the Part-time Member
Under-Graduate Medical Education Board
1
Maharashtra
Dr. Pallavi P. Saple
Post-Graduate Medical Education Board
1
Tamil Nadu
Dr. K. Senthil
Medical Assessment & Rating Board
1
Uttar Pradesh
Dr. Urmila Singh
Ethics & Medical Registration Board
1
Bihar
Dr. Sahajanand Prasad Singh
Selected Expert for Search Committee
S No
Name of State/ UT
Name of the Member
1
Odisha
Prof. Datteswar Hota
2 years 7 months ago
Editors pick,State News,News,Health news,Delhi,Hospital & Diagnostics,Doctor News,NMC News
Top five ophthalmic business items from 2022
This year’s top ophthalmic business article discussed ophthalmology’s venture into the metaverse.Read about this and other ophthalmic business news from 2022 below.Ophthalmology takes the plunge into the metaverseThe 2022 Digital Ophthalmic Society meeting was the first ever eye care conference to be held in a space station, or at least that is what it looked like.
Read more.Genentech voluntarily recalls Susvimo ocular implantGenentech is voluntarily recalling the Susvimo implant and insertion tool for the treatment of wet age-related macular degeneration in the U.S. Read more.
2 years 7 months ago
Medical News, Health News Latest, Medical News Today - Medical Dialogues |
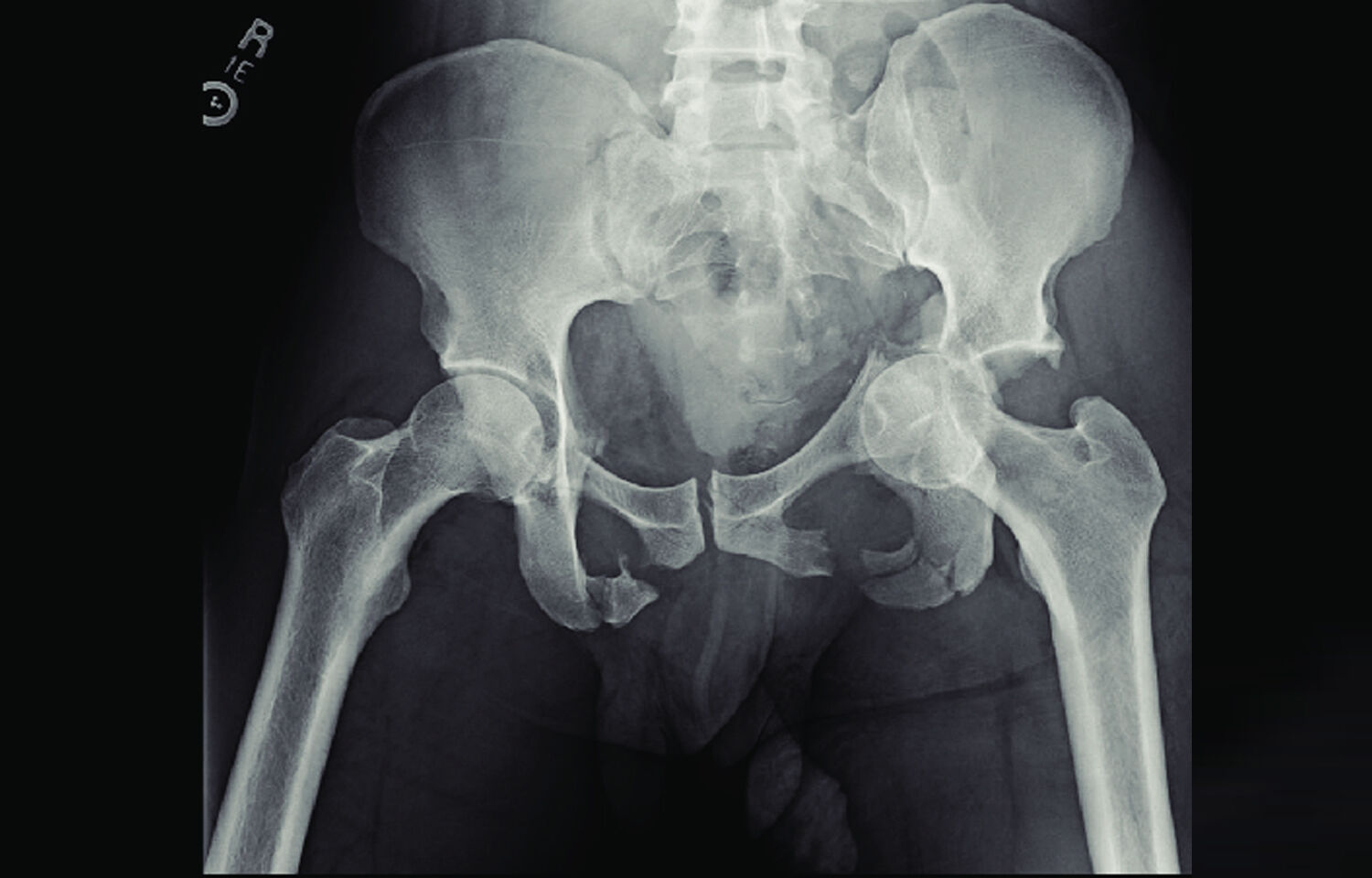
Treatment modalities of Hemorrhage control and mortality risk in unstable pelvic fractures
The mortality rate for patients with pelvic fractures has been studied extensively in the trauma literature, and most studies have placed it at 10%. Patients with pelvic fracture who required at least 4 units of blood transfusion and 1 significant hemorrhage control intervention were included in a recently published research that looked at their long-term prognosis.
Preperitoneal pelvic packing is associated with a greater risk of complications and a high overall mortality rate (36%), whereas angioembolization (AE) is associated with a decreased mortality rate (PP).
Patients with significant injuries to parts of the body other than the pelvis were also included in the study.
The authors performed a sensitivity analysis, excluding the subset of patients with an Abbreviated Injury Severity score of 2 or greater for head or chest, and confirmed their findings. The inclusion of these patients with a median Injury Severity Score of 24 may explain the high mortality rate and the median of 9 units of blood transfused. An independent risk of death has been linked to pelvic fractures in the context of other serious injuries, as shown by previous research. Perhaps most importantly, the authors show that there is substantial variation in the management of these critically ill patients across the United States, particularly in the choice and combination of interventions used, such as aortic endovascular balloon angioplasty (AE), preperitoneal PP, and resuscitative endovascular balloon angioplasty (REBOA).
This population-based research may have residual confounding, and patients who receive preperitoneal PP are physiologically different from those who can wait for the interventional radiology team, but the obvious issue from these findings is: what can we do to better rescue these patients and lower their high fatality rate?
The most noteworthy discovery of this research is the wide range of hospital management approaches. This variant warrants more investigation. Literature demonstrates that variance in procedures of care typically reflects variation in the quality of care offered, even if some variation is always necessary to provide patient-centered, tailored care.
2 years 7 months ago
Anesthesia,Orthopaedics,Surgery,Orthopaedics News,Top Medical News,Critical Care
Track your fitness progress
At the end of each holiday season, persons set out to create new goals for the coming year, as a new year presents a fresh start. Many health and exercise goals are created with the best of intentions but fall short in execution, as people often...
At the end of each holiday season, persons set out to create new goals for the coming year, as a new year presents a fresh start. Many health and exercise goals are created with the best of intentions but fall short in execution, as people often...
2 years 7 months ago
Risky living
HEALTH professionals are appealing to Jamaican men to monitor their health as more males suffer from elevated blood pressure and have a shorter life expectancy than women.
Although the Ministry of Health and Wellness was unable to provide data on the economic impact of men suffering from noncommunicable diseases (NCDs), it revealed that 24 per cent of men suffer from elevated blood pressure in comparison to 19 per cent of women.
"We find that men generally don't come to us, sometimes, until it is too late to do much about their illnesses. As to the reason for this, I am not sure. It could be cultural, or it could be the fact that many men believe they should always show that they are strong even when the occasion doesn't call for it," explained Dr Dwayne Hall, consultant general surgeon at Cornwall Regional Hospital.
Dr Hall noted that NCDs are those diseases not transferable by contact but rather developed through family genetics, degenerative changes, or unhealthy lifestyle habits, and argued that more men need to adopt better health-seeking behaviours because male life expectancy in Jamaica is 72 years while for women it is 76 years.
Health professionals have underscored that although more women in Jamaica suffer from NCDs than men, more males may actually be affected than the figures suggest.
"Generally, because females have better health-seeking behaviours it would appear as though females have a higher prevalence of noncommunicable diseases than men but this may not necessarily be the case — and this is why we are encouraging men to take monitoring their health seriously, especially as it relates to illnesses such as hypertension and diabetes," Dr Hall added.
The consultant general surgeon added that there are also misconceptions about medication and treatment for NCDs.
"Some Jamaicans have the false understanding that one month's supply of medication for hypertension and diabetes mellitus will cure the disease. They will additionally say, 'I'm not claiming this disease, doc. And, if I start medications I know I won't ever come off them, and this is not the life I want'," noted Dr Hall.
"Then, you have some Jamaican men who stay away from medications for hypertension as they say it affects their nature and make them ineffective. So, the hypertension will go unchecked for months, resulting in complications such as kidney failure, stroke and heart attacks.
Whole foods nutritionist Dr Elloreen Pryce explained that when it comes to NCDs and taking their health seriously, some men are often unwilling to seek, or follow medical advice.
"From my experience, many men do not take their health seriously," said Dr Pryce.
"When you tell them to check their prostate, especially if they're over 40, some will ask why it is important or make some excuse as to why they won't do it.
"They can be very difficult to work with when it comes to things that may impact their health positively. If you say to them, 'Eat more vegetables,' they may say they aren't rabbits or other animals. If you say to them, 'Cut down on the alcohol,' they will raise objections. In fact, in preparing their meal plans, if you say, 'Cut down on the meat,' they'll ask what you expect them to eat," added Dr Pryce, who also wants men to be more proactive when it comes to their health.
"There's an adage that says when you see men at the doctor, it's because they are extremely ill or were taken there by a woman. We want men to dispel this notion of not visiting the doctors until it is too late. We want them to take care of themselves so they can be around us for a long time," said Dr Pryce.
In the meantime, Hugh Reid, general manager of JN Life Insurance, pointed out that even when it comes to acquiring life insurance for protection against critical illnesses, men are less likely to purchase a policy than women.
"When we look at our data here at JN Life Insurance, women outnumber men two to one when it comes to our client base. We need men to take their health seriously because of the impact it has on our economy and families who lose their male breadwinners in the most productive years of their lives," said Reid.
Data from the Ministry of Health and Wellness have revealed that NCDs and injuries are a major public health burden in Jamaica, and are the leading cause of death.
In 2015 an estimated seven out of 10 Jamaicans died from the four major NCDs — cancer, cardiovascular disease, diabetes, and chronic lower respiratory disease.
The ministry adds that an individual suffering from NCDs spends approximately one third of the household per capita expenditure on health-care services and the purchase of pharmaceutical drugs.
2 years 7 months ago
Work more movement into your life!
It is almost the start of the new year, and time for a new you! You can do this by introducing more exercise into your life, but this is easier said than done when there is an ongoing pandemic, and the stresses of everyday life. Still, there are...
It is almost the start of the new year, and time for a new you! You can do this by introducing more exercise into your life, but this is easier said than done when there is an ongoing pandemic, and the stresses of everyday life. Still, there are...
2 years 7 months ago
PAHO/WHO | Pan American Health Organization
Institutions from Latin America and the Caribbean to receive grants to support the elimination of communicable diseases
Institutions from Latin America and the Caribbean to receive grants to support the elimination of communicable diseases
Cristina Mitchell
27 Dec 2022
Institutions from Latin America and the Caribbean to receive grants to support the elimination of communicable diseases
Cristina Mitchell
27 Dec 2022
2 years 7 months ago
2 tourists with Covid dismounted from cruise
A cruise ship that was sailing in the waters of the Caribbean Sea was forced to anchor in an emergency in recent days, in the Port of Sansouci in Santo Domingo, due to cases of Covid-19 detected on the vessel. It was reported that two tourists were admitted to the Abreu Clinic in the National District.
Only the fact that they are two males was provided, but the current state of the admitted passengers, as well as their nationality, are unknown, though it is assumed that they are foreigners.
Until now, no information has been released by the corresponding authorities, about the origin of the cruise and where the boat was heading, which according to information, has already left the Dominican port.
2 years 7 months ago
Health, World
Medical News, Health News Latest, Medical News Today - Medical Dialogues |
DrNB Clinical Haematology: Admissions, Medical Colleges, Fees, Eligibility Criteria details
DrNB Clinical Haematology or Doctorate of National Board in Clinical Haematology also known as DrNB in Clinical Haematology is a super specialty level course for doctors in India that is done by them after completion of their postgraduate medical degree course.
The duration of this super specialty course is 3 years, and it focuses on the study of the cause, prognosis, treatment, and prevention of blood-related diseases.
The course is a full-time course pursued at various accredited institutes/hospitals across the country. Some of the top accredited institutes/hospitals offering this course include Apollo Hospital-Gandhi Nagar, Army Hospital (R and R)-New Delhi, Dr. B L Kapur Memorial Hospital Pusa Road, New Delhi and more.
Admission to this course is done through the NEET-SS Entrance exam conducted by the National Board of Examinations, followed by counselling based on the scores of the exam that is conducted by DGHS/MCC/State Authorities.
The fee for pursuing DrNB (Clinical Haematology) varies from accredited institutes/hospital to hospital and may range from Rs. 80,000 to Rs. 4,00,000 per year.
After completion of their respective course, doctors can either join the job market or can pursue certificate courses and Fellowship programmes recognized by NMC and NBE. Candidates can take reputed jobs at positions as Senior residents, Consultants etc. with an approximate salary range of Rs. 5,50,000 toRs.19,00,000 per year.
DNB is equivalent to MD/MS/DM/MCh degrees awarded respectively in medical and surgical super specialities. The list of recognised qualifications awarded by the Board in various broad and super specialties as approved by the Government of India are included in the first schedule of the Indian medical council Act, 1956.
The Diplomate of National Board in broad-speciality qualifications and super speciality qualifications when granted in a medical institution with the attached hospital or in a hospital with the strength of five hundred or more beds, by the National Board of Examinations, shall be equivalent in all respects to the corresponding postgraduate qualification and the super-speciality qualification granted under the Act, but in all other cases, senior residency in a medical college for an additional period of one year shall be required for such qualification to be equivalent for the purposes of teaching also.
What is DrNB in Clinical Haematology?
Doctorate of National Board in ClinicalHaematology, also known as DrNB (Clinical Haematology) or DrNB in (ClinicalHaematology) is a three-year super specialty programme that candidates can pursue after completing a postgraduate degree.
Clinical Haematology is the branch of medical science dealing with the study of the cause, prognosis, treatment, and prevention of blood-related diseases.
National Board of Examinations (NBE) has released a curriculum for DrNB in Clinical Haematology.
The curriculum governs the education and training of DrNB in Clinical Haematology.
The postgraduate students must gain ample of knowledge and experience in the diagnosis, treatment of patients with acute, serious, and life-threatening medical and surgical diseases.
The PG education intends to create specialists who can contribute to high-quality health care and advances in science through research and training.
The required training done by a postgraduate specialist in the field of Clinical Haematologywould help the specialist to recognize the health needs of the community. The student should be competent to handle medical problems effectively and should be aware of the recent advances in their speciality.
The candidate is also expected to know the principles of research methodology and modes of the consulting library. The candidate should regularly attend conferences, workshops, and CMEs to upgrade her/ his knowledge.
Course Highlights
Here are some of the course highlights of DrNB in Clinical Haematology
Name of Course
DrNB in Clinical Haematology
Level
Doctorate
Duration of Course
Three years
Course Mode
Full Time
Minimum Academic Requirement
MD/DNB (General Medicine/ Paediatrics/ Biochemistry/ Pathology) obtained from any college/university recognized by the Medical Council of India (Now NMC)/NBE
Admission Process / Entrance Process / Entrance Modalities
Entrance Exam (NEET-SS)
INI CET for various AIIMS, PGIMER Chandigarh, JIPMER Puducherry, NIMHANS Bengaluru
Counselling by DGHS/MCC/State Authorities
Course Fees
Rs. 80,000 to Rs. 4,00,000 per year
Average Salary
Rs. 5,50,000 to Rs.19,00,000 per year
Eligibility Criteria
The eligibility criteria for DrNB in Clinical Haematology are defined as the set of rules or minimum prerequisites that aspirants must meet in order to be eligible for admission, which includes:
- Candidates must be in possession of a postgraduate medical Degree (MD/MS/DNB) from any college/university recognized by the MCI (Now NMC)/NBE.
-
The eligible feeder specialty qualification for DrNB in Clinical Haematology is mentioned below:
Name of Super Specialty course Course Type Prior Eligibility Requirement Clinical Haematology DM/DrNB MD/DNB (General Medicine) MD/DNB (Paediatrics) MD/DNB (Biochemistry) MD/DNB (Pathology)
•The prior entry qualifications shall be strictly in accordance with Post Graduate Medical Education Regulations, 2000 and its amendments notified by the NMC and any clarification issued from NMC in this regard.
•The candidate must have obtained permanent registration of any State Medical Council to be eligible for admission.
•The medical college's recognition cut-off dates for the Postgraduate Degree courses shall be as prescribed by the Medical Council of India (now NMC).
Admission Process
The admission process contains a few steps to be followed in order by the candidates for admission to DrNB in Clinical Haematology. Candidates can view the complete admission process for DrNB in ClinicalHaematology mentioned below:
- The NEET-SS or National Eligibility Entrance Test for Super specialty courses is a national-level master's level examination conducted by the NBE for admission to/MCh/DrNB Courses.
- Qualifying Criteria-Candidates placed at the 50th percentile or above shall be declared as qualified in the NEET-SS in their respective specialty.
- The following Medical institutions are not covered under centralized admissions for DM/MCh courses through NEET-SS:
1.AIIMS, New Delhi and other AIIMS
2.PGIMER, Chandigarh
3.JIPMER, Puducherry
4.NIMHANS, Bengaluru
- Candidates from all eligible feeder specialty subjects shall be required to appear in the question paper of the respective group, if they are willing to opt for a superspecialty course in any of the superspecialty courses covered in that group.
- A candidate can opt for appearing in the question papers of as many groups for which his/her Postgraduate specialty qualification is an eligible feeder qualification.
- By appearing in the question paper of a group and on qualifying the examination, a candidate shall be eligible to exercise his/her choices in the counseling only for those superspecialty subjects covered in said group for which his/ her broad specialty is an eligible feeder qualification.
Fees Structure
The fee structure for DrNB in Clinical Haematology varies from accredited institute/hospital to hospital. The fee is generally less for Government Institutes and more for private institutes. The average fee structure for DrNB in Clinical Haematology is around Rs. 80,000 to Rs. 4,00,000 per year.
Colleges offering DrNB in Clinical Haematology
There are various accredited institutes/hospitals across India that offer courses for pursuing DrNB in Clinical Haematology.
As per the National Board of Examinations website, the following accredited institutes/hospitals are offering DrNB (Clinical Haematology)courses for the academic year 2022-23.
Hospital/Institute
Specialty
No. of Accredited Seat(s) (Broad/Super/Fellowship)
Apollo Hospital International Plot No. 1A, GIDC Estate Bhat, District - Gandhi Nagar Gujarat-382428
Clinical Haematology
2
Apollo Multispecialty Hospitals Limited 58, Canal Circular Road, Kolkata West Bengal-700054
Clinical Haematology
1
Army Hospital (R and R) Delhi Cantt, New Delhi Delhi-110010
Clinical Haematology
2
Deenanath Mangeshkar Hospital and Research Centre. 8+13/2, Erandwane, Near Mhatre Bridge, Pune Maharashtra-411004
Clinical Haematology
1
Dr. B L Kapur Memorial Hospital Pusa Road, New Delhi Delhi-110005
Clinical Haematology
2
Fortis Memorial Research Institute Sector-44, Opposite HUDA CITY centre Metro Station, Gurgaon, Haryana-122002
Clinical Haematology
1
HealthCare Global Specialty Hospital (Formerly Bangalore Institute of Oncology) Deans Office #8, P. Kalinga Rao Road, Sampangiram Nagar, Bangalore Karnataka-560027
Clinical Haematology
1
Malabar Cancer Centre Moozhikkara P O, Kodiyeri, Thalassery, Kannur Kerala-670103
Clinical Haematology
2
Manipal Hospital No. 98, Rustum Bagh, Old Airport Road, Bangalore Karnataka-560017
Clinical Haematology
1
Narayana Hrudayalaya Hospital (NH-Narayana Health City, Bangalore) #258/A, Bommasandra Industrial Area, Anekal Taluk, Bangalore Karnataka-560099
Clinical Haematology
4
Rajiv Gandhi Cancer Institute and Research Centre Sec-5, Rohini, New Delhi Delhi-110085
Clinical Haematology
3
Sahyadri Super Specialty Hospital Plot No. 30C, Erandawane, Karve Road, Pune. Maharashtra-411004
Clinical Haematology
2
SCB Medical College and Hospital Mangalabag, Cuttack, Odisha Orissa Orissa-753010
Clinical Haematology
2
Sir Ganga Ram Hospital Rajinder Nagar, New Delhi Delhi-110060
Clinical Haematology
2
St. Johns Medical College Hospital Sarjapur Road, Koramanagala Bangalore Karnataka-560034
Clinical Haematology
2
Tata Medical Center 14 Major Arterial Road (E-W), Newtown, Rajarhat, Kolkata West Bengal-700160
Clinical Haematology
2
Yashoda Super Speciality Hospital Raj Bhavan Road, Somajiguda, Hyderabad Telangana-500082
Clinical Haematology
1
Syllabus
A DrNBin Clinical Haematology is a three years specialization course that provides training in the stream of ClinicalHaematology.
The course content for DrNB in Clinical Haematology is given in the NBE Curriculumreleased by the National Board of Examinations, which can be assessed through the link mentioned below:
DrNB Clinical Haematology In India: Check Out NBE Released Curriculum
1. THEORY SYLLABUS: Departments involved in the training programme:
i. Clinical Haematology (Adult and Pediatric) and HSCT
ii. Laboratory Haematology including Haematopathology, Cytogenetics and Molecular genetics
iii. Transfusion Medicine
iv. Microbiology
v. Biochemistry
vi. Pathology
vii. Nuclear Medicine
viii. Radiotherapy
ix. HLA/transplant immunology
2. CLINICAL HAEMATOLOGY TRAINING:
Under the faculty's guidance and supervision, the postdoctoral student will be responsible for the acquisition of knowledge in all areas of Haematology (clinical and laboratory) and Transfusion Medicine. Such knowledge will be acquired through bedside teaching, seminars, case presentations, journal clubs, tutorials, proper use of the library, and formal reviews of selected major topics. Faculty should be present at various exercises to provide appropriate input. The trainee will acquire clinical experience by day-today management of all patients admitted to the Haematology service under the faculty's supervision.
i. Basic Haematology:
a. Cell Cycle and haematopoiesis, iron, vitamin B12 and folate metabolism, concepts of coagulation and natural anticoagulant, structure, and functions of all types of blood cells.
b. Principles of chemotherapy, concepts of combination chemotherapy, their toxicities.
c. Monoclonal antibodies, immunotherapy and small molecules in Haematology, their use and toxicities.
d. Immunology: principles of innate and adaptive immunity and transplant immunology.
ii. Disorders of Red Cell: Clinical evaluation of a patient with anemia, adequate history taking, clinical examination, appropriate laboratory investigations, and management.
a. Iron deficiency anemia: Iron metabolism and its regulation, pathophysiology of iron deficiency, epidemiology, iron deficiency as a community health program, causes in the population, control strategies in the population. Interpretation of serum iron, TIBC, transferrin, ferritin to diagnose iron deficiency. Relevant test to establish the cause of the iron deficiency. Management, including iron replacement and treatment of the underlying cause. Epidemiological significance of iron deficiency anemia in the population and preventive strategies.
b. Vitamin B12 and folate deficiency: Understanding the role of Vitamin B12 and folate in cellular metabolism and the interaction of disease and drugs with B12 and folate metabolism. Clinical and laboratory evaluation of the deficiency and management of vitamin B12 and folate deficiency.
iii. Haemolyticanaemia:
a. Thalassemia and Haemoglobinopathies: Genetic basis and pathophysiology of the disorder, clinical and laboratory evaluation of the patient, with their management, and long-term follow-up. Adequate knowledge on transfusion regimes, chelation, thalassemia complications, the role of splenectomy, and HSCT. Principles of control of the thalassemia syndromes in the population, screening strategies, antenatal diagnosis, genetic counseling and monitoring of complications due to iron overload.
b. Sickle cell disease: Pathophysiology, evaluation, management of the steady-state as well as various sickle cell crises and management of chronic complications. Clinical and haematological features of the various sickle cell diseases. Therapeutic role of HSCT.
c. Inherited enzymopathies (Red cell G6PD deficiency & others) and membrane opathies: evaluation, planning and interpretation of investigations (like Osmotic Fragility Test and Eosin-5'-Maleimide dye binding test) to ascertain the diagnosis, and management. The precise role of splenectomy in the present era and emphasis on genetic counseling.
d. Acquired Haemolytic disorders: evaluation and management of acquired haemolytic anemia, the role of immunosuppression, intravenous immunoglobulin, plasmapheresis and role of splenectomy.
e. Management of rare congenital and acquired red cell disorders like porphyria, congenital dyserythropoietic anemia, pure red cell aplasia (inherited and acquired), side roblastic anemias, and nonspherocytichaemolytic anemia etc.
iv. Disorder of White Cell:
a. Neutropaenia: Clinical evaluation of the neutropenic patient, role of surveillance microbiology, antimicrobial therapy in neutropenia with emphasis on the multidrug-resistant organism, role of growth factors, barrier nursing, and principles of providing a sterile environment for the neutropenic patient. Evaluation and management of inherited neutrophil disorders.
b. Functional disorders of neutrophils: laboratory tests for evaluating neutrophil dysfunction, and the role of growth factors, antimicrobial prophylaxis, and HSCT in its management.
c. Leukemia (acute and chronic): Clinical evaluation, diagnostic confirmation by morphology, immunopheno typing, special stains, cytogenetics, and molecular genetics. They should know the algorithmic approach in immunopheno typing for diagnosis of leukemia's. The trainee must be familiar with the principles of leukemia management and standard protocols available. They should understand the pharmacology of chemotherapeutic drugs, their mode of administration, toxicity and complications such as extravasation. They should have knowledge of supportive care, including transfusion support in managing patients with all types of leukemia. The trainee should be familiar with the management of complications like hyper leukocytosis, tumor lysis syndrome and drug toxicities.
d. Myeloproliferative neoplasms (MPN): Classification, systematic diagnostic evaluation of MPNs, risk stratification, and current management strategies, including the role of HSCT.
e. Myelodysplastic syndrome (MDS): Clinical evaluation, diagnosis, risk stratification, and management, including the role of supportive care and HSCT.
f. Lymphoma: WHO classification of lymphomas, clinical evaluation, principles of diagnosis, and staging. Immunophenotypic (flow cytometry and immunohistochemistry) approach to diagnosis of lymphoproliferative disorders, role of cytogenetic and molecular tests in diagnosis and prognostication of lymphomas. Management of the different types of lymphomas including chemotherapy, HSCT, maintenance therapy and follow-up.
g. Multiple Myeloma and other Para protein disorders: Clinical, laboratory and radiological evaluation of a patient with plasma cell disorders. Interpretation of electrophoresis and imaging reports, assessment of endorgan damage, role of flow cytometry, cytogenetics and risk stratification in diagnosis and management. Treatment algorithm of plasma cell dyscrasia and response assessment. Role of HSCT, post-transplant consolidation, maintenance therapy, and follow-up. Management of complications like anaemia, renal failure, hypercalcemia, infections, bone disease and hyper viscosity. Concepts of monoclonal gammopathy of undetermined/renal/clinical significance. Evaluation and treatment of Waldenstrom'smacroglobulinemia and other rare para proteinemias.
h. Immunodeficiency disorders: Trainees must be able to investigate and manage primary immunodeficiency disorder systematically. They should have adequate knowledge of immunoglobulin replacement principles, interferons, growth factors, antibiotic prophylaxis, and role HSCT. They should have adequate knowledge on the haematological manifestations of acquired immunodeficiency disorders and its management.
i. Disorders of histiocytic: Evaluation and management of Haemophagocyticlymphohistiocytosis and histiocytic malignancies, Langerhans cell history to is and storage disorders.
v. Pancytopenia:
a. Aplasticanaemia: Etiology, pathophysiology, evaluation, and management, including immune suppression (anti-thymocyte globulin, cyclosporine), eltrombopag, and supportive therapy. Role of HSCT including the role of haploidentical transplant. Management of a relapsed case of aplastic anaemia.
b. Bone marrow failure syndrome (BMFS): Etiology, classification, pathophysiology, clinical features of various bone marrow failure syndromes. Clinical evaluation and investigations including the role of cytogenetics, stress cytogenetics and relevant molecular workup for confirmation of the diagnosis. Knowledge of telomeropathies and ribosomopathies and their management. Therapeutic strategies for various BMFS with curative treatment options of HSCT and role of supportive care
c. Evaluation and management of pancytopenia due to other systemic disorders, drugs, autoimmune disorders and sepsis.
vi. Haemostasis and thrombosis:
a. Trainees should be thorough with the clinical and laboratory approach to a patient with a bleeding tendency.
b. Thrombocytopaenia: Evaluation and investigation of the cause of thrombocytopaenia and its management.
c. Inherited platelet function disorders: Clinical evaluation, laboratory diagnostic strategies, and management. Interpretation of platelet aggregation studies, flow cytometry and viscoelastic tests for platelet defects.
d. Inherited coagulation factor deficiencies: Clinical evaluation and laboratory diagnosis of haemophilia, principles of factor replacement, prophylaxis strategies and on-demand therapy, replacement schedule in a person with haemophilia who needs surgery, in the event of major bleed or trauma, and management of complications of haemophilia including arthropathies. Concepts of development of inhibitor and interpretation of inhibitor assay. Principles of managing patients with inhibitors including management of breakthrough bleeds.
e. Acquired bleeding disorders: Evaluation and management of DIC, haemorrhagic complications of liver disease, renal failure, acquired coagulation factor deficiency and drug related platelet disorder. Management of thrombocytopenia in pregnancy.
f. Thrombotic disorders: Classification and laboratory diagnosis of inherited thrombotic disorders, evaluation of acquired thrombotic disorders with emphasis on cancer related thrombosis, the clinical use of anticoagulants, duration of therapy, and monitoring emphasizing the upcoming role of DOACs.
vii. Haematopoietic stem cell transplantation (HSCT):
a. Indication sand outcome of HSCT in various diseases. Role of autologous and allogenic transplant in different diseases. Indications and outcome of HLA matched sibling donor, matched unrelated donor, cord blood and haploidentical transplant in different diseases.
b. Thorough knowledge on donor selection.
c. Conditioning regimens used for different disease. Strategies for GvHD prevention.
d. Peripheral blood and bone marrow harvest of stem cell and its manipulation, cryopreservation.
e. Supportive care and management of complications in the post-transplant period.
f. Monitoring and management of the long-term complications in posttransplant patients.
g. Post-transplant vaccination.
h. Post-transplant immune reconstitution and interpretation of chimerism studies.
viii. Consultation Haematology:
a. Haematological complications of pregnancy.
b. Haematological complications of systemic disease.
c. Haematological problems of the intensive care patient.
d. Drugs-related haematological issues.
e. Haematological problems in the newborn.
f. Consults in rheumatology – APS/ HLH/ MAS/ CAPS
g. Haematological consults in geriatric medicine
h. Haematological manifestations in solid malignancies e.g. myelopthisic anemia, cancer related thrombosis.
ix. Supportive care:
a. Management of nausea, vomiting, diarrhoea.
b. Pain management.
c. Management of cytopaenia and its complications like infections, bleeding, and anaemia.
d. Gonad preservation.
e. Parenteral and enteral nutritional support, diet.
f. Infection control, environmental measures, hygiene.
x. Recent Advances in Haematology:
a. Recent concepts on iron metabolism, coagulation, and other basic aspects of Haematology.
b. Recent advances in molecular biology in Haematology.
c. Modern diagnostic tools in Haematology.
d. Recent advances in the understanding of haematological diseases.
e. New drugs in Haematology, including monoclonal antibodies, targeted therapy, and small molecules
f. Management of multidrug resistant organisms and newer antimicrobials.
g. New developments and upcoming role of imaging in Haematology
h. Advances in HSCT, CAR-T cell therapy, and gene therapy.
i. New developments in Haematology as discussed in yearly international conferences and webinars.
xi. Transfusion Medicine:
a. Blood component preparation and clinical use: Blood collection, knowledge on anticoagulants used in storage and their effect on storage. Component preparation and storage. Quality assurance in transfusion medicine.
b. A thorough understanding of the clinical indications for the proper use of specific blood components.
c. Diagnosis and management of transfusion associated complications.
d. Concepts and indication of leucodepletion and irradiation of blood components. Knowledge on the performance of the same.
e. Screening and management of allo-immunisation concerning transfusion.
f. Principles of the plasmapheresis. Principles of the machine, continuous versus intermittent flow techniques, replacement fluids for plasmapheresis, current status, and indication in various diseases should also be known and understood.
xii. Bioethics:
a. Respect human life and the dignity of every individual.
b. Refrain from supporting or committing crimes against humanity and condemn all such acts.
c. Treat the sick and injured with competence and compassion and without prejudice and apply the knowledge and skills when needed.
d. Protect the privacy and confidentiality of those for whom we care and breach that confidence only when keeping it would seriously threaten their health and safety or that of others.
e. Work freely with colleagues to discover, develop, and promote advances in medicine and public health that ameliorate suffering and contribute to human well being
f. Educate the public about the present and future threats to the health of humanity.
g. Advocate for social, economic, educational, and political changes that ameliorate suffering and contribute to human wellbeing.
h. Teach and mentor those who follow us, for they are the future of our caring profession.
xiii. Research and biostatistics: Clinical trial protocol designing, Clinical epidemiology, Biostatistics, Bioethics, and Medico-legal issues pertaining to study patients.
3. LABORATORY HAEMATOLOGY:
i. Laboratory Equipment's and organization:
a. Proper use and care of common laboratory instruments such as the light microscope, centrifuge, water baths, freezers, etc.
b. Trainee must have adequate knowledge of all laboratory equipment's essential maintenance, including their calibration procedure and frequency.
c. Knowledge on setting up a Haematology laboratory, its workflow procedures, handling, storage, and sample disposal.
d. Technical and non-technical personnel requirements, their periodic training, and safety.
e. Maintenance of record, data preservation, and generation of laboratory statistics.
f. Quality assurance (Internal and External) measures and assessment of preanalytical, analytical, and post-analytical variables. Period audits to ensure precision and accuracy of lab results.
ii. Basics of Laboratory Haematology
a. Blood collection of samples by venipuncture and finger prick methods.
b. Knowledge about the types of vacutainers and anticoagulants used for sample collection, the ratio of sample to the anticoagulant, the effects of delay in sample processing, and proper temperature of sample storage.
c. Determination of blood counts (haemoglobin, haematocrit and other red cell indices, total and differential WBC counts andplatelet count) manually.
d. Use of automated electronic blood cell counters, including principles and practice. Interpretation of the parameters of advanced cell counters.
e. Preparation, staining, and interpretation of peripheral blood smears.
f. Review of normal and abnormal blood smears with emphasis on:
Morphology of red cells, white cells, and platelets.
Performance of WBC differential count.
Subjective assessment of platelet count.
Interpretation of abnormal smear to ascertain approach to diagnosis.
g. Supravitally staining of reticulocytes: manual and automated techniques and interpretation of the results.
h. Performance of bone marrow aspiration and trephine needle biopsy.
i. Preparation of smears of bone marrow aspirates and biopsy imprints (touch preparations) and their staining by Romano sky stain as well as special stains like Perl's stain, PAS, Sudan Black B, Myeloperoxidase, Specific, on-specific and Dual esterase.
j. Performance and interpretation of HbS (sickle hemoglobin) solubility test, screening for red cell G6PD activity and its interpretation.
iii. Laboratory Investigation of HaemolyticAnaemias:Red cell membrane disorders and Immune Haemolyticanaemias:
a. Quantitation of normal HbA, HbF, HbA2 and abnormal HbS,HbD,HbE,HbC, etc., by electrophoresis and chromatography.
b. Screening for unstable haemoglobin (heat instability and Isopropanol tests).
c. Supravital staining for HbH inclusions.
d. Standard hypotonic saline osmotic fragility test, incubated osmotic fragility test and Eosin-5'-Maleimide binding test by flow cytometry.
e. Heinz body preparation.
f. Screening for red cell G6PD deficiency and quantitative estimation of red cellG6PD activity.
g. Screening for red cell pyruvate kinase (PK) deficiency and assay of red cell pyruvate kinase activity.
h. Screening for other red cell enzymopathies.
i. PNH flow cytometry and FLAER for PNH, Urine haemosiderin.
j. Direct and indirect anti-globulin (Coombs) tests, warm and cold autoantibody (Cold agglutinin) titre, determination of thermal amplitude of cold agglutinin.
k. Role of flow cytometry in the evaluation of Haemolyticanaemia.
l. Role of molecular techniques including NGS in the diagnosis of Haemolyticanaemia.
m. Sickling test.
Miscellaneous biochemical tests on Red cells, Plasma, and Urine:
a. Examination of urine red cells, haemosiderin, haemoglobin, urobilinogen, and bilirubin.
b. Principles of estimation and significance of serum ferritin, iron, TIBC, serum cobalamin, red cell folate, serum folate, cry globulin.
iv. Laboratory Investigation of Bleeding Disorders:
Investigation of platelets disorders:
a. Performance of platelet count and morphology, ivy bleeding time, and template bleeding time. Interpretation of MPV and IPF in patients with low platelet counts.
b. Principles, practice, and interpretation of platelet aggregation study and thromboelastographic.
c. Understand the technique and use of flow cytometry in the diagnosis of platelet disorders.
d. Laboratory evaluation of suspected heparin-induced thrombocytopenia (HIT).
Screening and diagnosis of coagulation factor abnormalities:
a. Prothrombin time (PT), activated partial thromboplastin time (APTT), thrombin time (TT).
b. Plasma fibrinogen assay, differentiation of afibrinogenaemia, and dysfibrinogenemia.
c. FDP and D- Dimers
d. Correction studies (Mixing studies) with normal plasma, and factor deficient plasma. APTT based inhibitor screen assay for both immediate acting inhibitor and time dependent inhibitors.
e. Assays of clotting factors with particular emphasis on factors VIII and IX.
f. Urea solubility test and an assay of factor XIII
g. Screening for inhibitors against coagulation factor, especially factor VIII and IX, titration of inhibitor by Bethesda assay.
Relevant tests of fibrinolytic activity:
a. Laboratory Investigation of Thrombotic disorders:
Assays of plasma Antithrombin, protein C, protein Sand Activated Protein C resistance for factor V Leiden.
Principles of screening tests and interpretation of results for lupus anticoagulant by dRVVT as well as anticardiolipin and antiβ2glycoprotein-1 antibodies.
Laboratory monitoring of anticoagulant (heparin and direct oral anticoagulant) therapy: Anti-Xa activity diluted Thrombin Time, and Ecarin clotting time. Diagnosis of Heparin induced thrombocytopenia.
Molecular tests for diagnosis of thrombophilia like Factor V Leiden,
Prothrombin P20210A, MTHFR mutation etc.
b. Flow Cytometry: The trainee should be well versed with the principle of flow cytometry and- flow cytometer's functioning. They must be thorough with the procedure's sample requirements, processing, and analysis of the results. They should be well-versed in the interpretation of flow cytometry results for the diagnosis of haematological malignancies. They must also understand the role of a flow cytometer in evaluating red cell and platelet disorders.
c. Cytogenetics: Understanding the principle and technique of cytogenetics (particularly conventional karyotype and fluorescence in-situ hybridization), relevance, and significance of chromosomal studies in the context of various diseases.
d. Molecular Biology: Understanding the principle involved in the molecular diagnosis of hematological disorders:
DNA and RNA extraction.
RT-PCR and RQ-PCR.
RFLP and other techniques to evaluate polymorphisms.
Difference methods of mutation detection, their principle, and technique.
DNA Sequencing and fragment length analysis for monitoring response to therapy.
e. Transfusion Medicine:
Basic laboratory aspect of transfusion medicine:
ABO blood grouping (forward and reverse), Rh typing Wof donors and recipient's indirect ant globulin test), antibody identification following elution by various techniques.
Blood group compatibility (cross-matching).
Investigation of ABO, Rh, and another immune-Haemolytic disease of the newborn.
Investigations of platelet refractoriness and heparin-induced thrombocytopenia.
Donor recruitment, their clinical and laboratory evaluation before phlebotomy.
Principles of phlebotomy.
Blood component preparation and storage.
Practical and documentation procedures involved in issuing and transfusing blood and cellular components.
Principles and mechanics of blood component preparation.
Principles of apheresis and performance of the procedure concerning the collection of platelets, granulocyte, and stem cells.
Principle and performance of plasmapheresis.
Practical steps in the laboratory investigation of transfusion reactions.
f. Histopathology: Practical laboratory training and related theory should cover the following areas:
Tissue processing (particularly trephine biopsy and lymph nodes)
Techniques of cytology, including cytosine concerning body fluid, CSF in particular.
g. Knowledge in anatomic pathology and immunohistochemistry relevant to the diagnosis of the hematological disorder.
h. Biochemistry: Knowledge of the principle, technique, and interpretation of immunoassays, electrophoresis, nephelometry, etc. The role of proper and adequate sample collection and transport for the tests.
i. HLA module: understanding the principles of:
• Separation of lymphocytes using density gradient centrifugation.
• The micro-lymph cytotoxicity test and its application in HLA typing, cross-matching, and antibody screening.
• DNA-based HLA typing, including high-resolution HLA typing using next-generation sequencing.
• HLA antibody identification.
j. Nuclear Medicine: Principle of PET scan and its role in diagnosis, response assessment, and monitoring of haematological disorders
k. Radiation Oncology: The students should be encouraged to learn about radiotherapy basics and have hands-on training on linear accelerator, IGRT, IMRT, TBI, CRRT in haemato-oncological practice and blood components radiation.
Career Options
After completing a DrNB in Clinical Haematology, candidates will get employment opportunities in Government as well as in the Private sector.
In the Government sector, candidates have various options to choose from which include Registrar, SeniorResident, Demonstrator, Tutor etc.
While in the Private sector the options include Resident Doctor, Consultant, Visiting Consultant (ClinicalHaematology), Junior Consultant, Senior Consultant (Clinical Haematology),Critical Care Specialist, etc.
Courses After DrNBin Clinical Haematology Course
DrNB in Clinical Haematology is a specialisation course that can be pursued after finishing a Postgraduate medical course. After pursuing specialisation in DrNB in ClinicalHaematology, a candidate could also pursue certificate courses and Fellowship programmes recognized by NMC and NBE, where DrNB in Clinical Haematology is a feeder qualification.
Frequently Asked Question (FAQs) – DrNBin Clinical Haematology Course
Question: What is the full form of DrNB?
Answer: The full form of DrNB is a Doctorate of National Board.
Question: What is a DrNB in Clinical Haematology?
Answer: DrNB Clinical Haematology or Doctorate of National Board in Clinical Haematology also known as DrNBin Clinical Haematology is a super specialty level course for doctors in India that is done by them after completion of their postgraduate medical degree course.
Question: What is the duration of a DrNB in ClinicalHaematology?
Answer: DrNB in Clinical Haematology is a super specialty programme of three years.
Question: What is the eligibility of a DrNB in Clinical Haematology?
Answer: Candidates must be in possession of an MD/DNB (General Medicine/ Paediatrics/ Biochemistry/ Pathology) from any college/university recognized by the Medical Council of India (now NMC)/NBE.
Question: What is the scope of a DrNB in ClinicalHaematology?
Answer: DrNB in Clinical Haematology offers candidates various employment opportunities and career prospects.
Question: What is the average salary for a DrNB in Clinical Haematology candidate?
Answer: The DrNB in Clinical Haematology candidate's average salary is between Rs.5,50,000 to Rs. 19,00,000 per annum depending on the experience.
Question: Can you teach after completing DrNB Course?
Answer: Yes, candidate can teach in a medical college/hospitalafter completing a DrNB course.
2 years 7 months ago
News,Health news,NBE News,Medical Education,Medical Colleges News,Medical Courses News,Medical Universities News,Medical Admission News,Latest Medical Education News,Medical Courses
HF prevalence may be higher than estimates in low- to middle-income countries
The age-standardized prevalence of HF in low- to middle-income countries may be much higher than modeling estimates suggest and signals the persistence of global CVD health disparities, according to researchers.“Our data underscore that HF is a likely an underrecognized cardiovascular disease and health disparity, given the difference in modeling estimates as compared to our population-based da
ta and given the difference in prevalence and age of onset among this Haitian cohort as compared to higher-income settings,” Justin R. Kingery, MD, PhD, associate professor of medicine at
2 years 7 months ago
Avoiding Christmas colic
COLIC, which can impact adults, is frequently related with babies who cry a lot. Colic is frequently described in adults as an abrupt gastrointestinal or urination pain that gradually gets better.
According to general, laparoscopic and bariatric surgeon Dr Alfred Dawes, localised, intermittent discomfort in the bladder or abdomen is the primary sign of colic.
Dr Dawes said colic happens when a hollow internal body organ, such as the intestines, gall bladder, rectum, kidneys, or ureters, becomes blocked. He said, the muscles around the impediment contract vigorously in an effort to remove it, which results in painful spasms and gallstones and kidney stones are two of the blockages that cause colic most frequently. In addition, he said sometimes it is actual faeces that casues what is termed as a pseudo or false obstrcution and when trying to pass hard faeces (from overeating or not drinking enough water) the cramping pain starts and comes in waves.
"An acute discomfort that progressively lessens might continue for up to five hours during a colic episode. A lingering discomfort may last for up to 24 hours. A person is more likely to experience further episodes of colic after one," he said.
Moreover, during the Christmastime, it is customary for individuals to experience colic often caused from overeating and gas from foods eaten, for example, dairy if lactose intolerant and flour for those with gluten intolerance.
So while we enjoy the likes of our hams, variety of meats, savouries, sweets, and delicious treats we don't have year-round, be mindful not to overdo it or take risks and end up with an uncomfortable ending to what should be a day of festivities.
Below Dr Dawes shares ways to prevent colic and in the event it happens, several treatments and home remedies.
Prevention
The key is to take action to maintain the health of your digestive system. Among the actions to take are:
Eating a diet high in fibre (that means plenty of fruits, vegetables, and whole grains)
Maintaining hydration
Avoiding foods high in fat
Losing weight if necessary
At-home remedies for colic episodes include:
Keeping hydrated by drinking lots of water
Taking ibuprofen or paracetamol to ease pain
Applying a hot water bottle to the sore spot to relieve pain
Rub or lightly massage the afflicted region
Following a colic diagnosis, a doctor might suggest one of the following treatments:
Pharmaceuticals to treat illnesses, anti-inflammatory treatments, and painkillers to alleviate symptoms
Surgery to explore intestinal obstructions, remove kidney stones, or remove the gallbladder
Stone-melting medications shock-wave therapy, which can shatter stones into small pieces
When to seek medical help
The majority of colic episodes end within a few hours, but if they persist frequently, it is preferable to see a doctor for a diagnosis.
Anyone exhibiting any of the following signs and symptoms ought to consult a doctor immediately:
Jaundice (yellowing of the skin and whites of the eyes) (yellowing of the skin and whites of the eyes)
Long-lasting abdominal discomfort or abdominal pain that is so severe that it is impossible to find relief from it in any position
Cold and a high temperature
A quick heartbeat
Being unable to drink without throwing up
Continual vomiting
Moreover, Dr Dawes said colic comes in waves of pain that comes and goes, therefore any pain that is constant and unremitting can be a sign of something serious and should never be attributed to colic.
2 years 7 months ago
Utilising telemedicine during the holidays
THE excitement and anticipation for the most festive time of the year often cloud our thoughts into not anticipating any accidents, mishaps or illnesses — although these are all very common during the season.
Nevertheless, your holiday can still run smoothly if you utilise resources such as telemedicine — doctors available to you online via phone call, video call or text messaging. Whether this flu season causes you to get sick, your seasonal allergies get worse, an accident happens while prepping for the holidays or any other non-emergent mishap, you can turn to digital health-care platforms, such as MDLink, for safe, convenient and reliable services,
Keep reading to understand how you can count on telemedicine services this holiday.
How telemedicine can be useful this holiday
• Helps to avoid the holiday traffic. While telemedicine allows you to avoid long waits in the doctor's office and pharmacy, you may still get caught up in the holiday rush. This can include increased traffic as well as crowding on public transportation. Instead, speak with a specialist online from the comfort of your home, or wherever you may be, through platforms such as MDLink — helping you to avoid the roads as much as possible.
•Facilitates treatment from familiar providers during travel. Whether you're travelling locally or abroad, you can use MDLink's platform anywhere that has access to the Internet — allowing you access to your local health-care provider(s) who are aware of your medical history and can provide diagnosis/treatment within minutes virtually. Additionally, if you are in a rural area where the nearest health-care facility is not nearby, you can use this platform to access immediate health care without having to travel a far distance.
• Monitoring and care for chronic illnesses. Most take time off during the holiday season, but your chronic illnesses does not. Whether you have a specific concern about your illness, need to do a routine check-up or have a monthly prescription refilled, telemedicine can assist you to get all this done without running the risk of further complications.
When not to use telemedicine over the holidays
While telemedicine is extremely convenient and will prove to be a useful tool for many this holiday, there are some instances where this form of treatment is not appropriate. If you have any of the following symptoms please visit an urgent care facility immediately:
•Excess bleeding and/or vomiting
• Falling unconscious or severe head trauma
• Breaking or fracturing a body part
• Severe allergic reactions
• Emergent flare-ups of chronic illnesses (such as lupus, cancer, diabetes, etc)
• Severe chest pain
Additionally, if you do choose to contact a doctor via telemedicine for an accident such as a fracture, for example, they may send you a referral to go to an in-person facility to get some X-rays done. If your doctor online suggests that you get in-person care, please do so immediately.
We hope for everyone a safe, enjoyable, and accident-free holiday. However, if anything does happen, know that you can count on MDLink wherever you are and whenever you need medical advice.
Dr Ché Bowen, a digital health entrepreneur and family physician, is the CEO & founder of MDLink, a digital health company that provides telemedicine options. Check out the company's website at
www.theMDLink.com. You can also contact him at drchebowen@themdlink.com.
2 years 7 months ago
Shake the salt this Christmas
TIS the season for overindulgence.
Christmas Day has the potential to drastically increase our salt intake! With pre-lunch snacks, canapés, eggnog, home-made chocolate, peppermint, maple-glazed ham, and a Christmas dinner that includes a starter, main dish, and dessert, food plays a prominent role in the celebrations. There are endless opportunities for us to satisfy our cravings. But could all these treats harm our long-term health?
These items can all have up to 15.7 grams of salt in them, which is more than twice the daily recommended limit of six grams.
But with a few quick tricks and time-saving techniques, you can cut the salt on your Christmas menu by up to 10 grams (5.7 grams of salt). The American Heart Association advises consuming no more than two-thirds teaspoons of salt each day. In fact, today, American adults consume nearly 50 more sodium than the limit recommended by federal guidelines, putting us at risk of high blood pressure. Left unaddressed, consultant urologist Dr Jeremy Thomas says this can increase our likelihood of experiencing kidney disease, stroke and heart disease – the country's leading cause of death.
So, does this mean we need to forget our upcoming feasts? Fortunately, no. Dr Thomas shares tips on how to reduce our salt intakes this Christmas and why it is necessary to do so.
1. Do away with the salt shaker: If it's not there, we can't use it. By taking the salt shaker off the table and out of the kitchen cupboard, you can lessen the temptation to over salt.
2. Avoid items high in sodium: Avoid the high-sodium bottled sauces and marinades, soy sauce, broth, garlic salt, onion salt, and other seasoning. Instead, add flavour to food with ingredients like fresh herbs, spices, vinegar, lemon, garlic, and onions.
3. Steer clear of ultra-processed foods and fast food: The FDA estimates that eating packaged, commercially produced, or restaurant items accounts for more than 70 per cent of Americans' dietary sodium intake. Whenever possible, opt for fresh foods or ingredients with no added salt.
4. Examine the packaging: Choose foods with no more than the recommended nutritional value, check brand websites or package labels. Be sure to check labels when purchasing the ingredients for your meals.The salt content of similar foods can vary greatly, so it's a good idea to check the label, especially on snacks like crisps, olives, and nuts. By selecting the lesser salt options that are offered, you can also save over a gram in a starting of smoked salmon, cream cheese, and bread.
5. Cook at home: Making a roast from scratch at home will significantly reduce the salt content. Although ready-made vegetables seem like a time-saving option, they can include excessive amounts of salt. In contrast, home-cooked veggies without salt added contain only a trace. Another way to reduce salt consumption is to buy a fresh or frozen turkey or ham and cook it at home; pre-prepared portions frequently contain a lot of salt. Use herbs like rosemary, cinnamon, and cloves in place of salt or butter to add flavour. Make sure to rinse the food before cooking and serving if you're using canned goods. Remember to include fruits and veggies on half of your plate.
6. Time-savers: There are a number of foods which are low in salt or don't typically vary between brands so you can save your time and buy these foods. By selecting smaller-sized holiday goodies, you can also cut back on your sodium intake. When dining out, request sauces and gravies on the side rather than putting them on top of your food.
Dr Thomas added: "About one in three Jamaicans or 33 per cent live with hypertension or some form of cardiovascular disease. It is endemic and the number one killer in Jamaica, worse than crime. However, it is not something that happens overnight, it takes time to develop and so lifestyle changes can prevent, slow the progression or help maintain control. So while we might let go our diets for the Christmas season, we need to be aware not to overdo it and to mind how much we veer to indulge. Reduce the salt and sugar and still try to get some exercise in."
2 years 7 months ago
Tips for keeping heart disease at bay for the holidays
HEART disease is the last thing on people's minds at this jolly time of the year. We want to be in a happy and joyful mood surrounded by friends and family, and fun and laughter. Any distractions that may interrupt this mood are most unwelcome.
The unfortunate reality, however, is that for some individuals, chronic illness may exacerbate, and sudden illness may occur. Top on this list is cardiovascular diseases which remain the top causes of death and disability in most countries including Jamaica. Studies have shown that cardiovascular problems occur more frequently during the end of year festivities, peaking in the new year. Hypertension, for example, is a leading risk factor for heart attack and stroke. To enter the holidays in good health and stay in good health, it is prudent to keep your blood pressure under control during the holidays.
But we can play a role in keeping heart disease at bay during the holidays. How can we do that? By taking precautionary measures to limit or risk and control our risks.
Don't eat with your eyes
During the holiday period, most of us will be out of work and exposed to a lot more food and beverages than usual. We are also likely to exercise less. It is okay to party and have fun but be mindful of what goes into your mouth, especially if you have high blood pressure, diabetes, or heart failure. A good habit to help you along is to have a heart healthy meal at home before stepping out so you would be less likely to overindulge. A vegetable tray is almost always a good idea but be cautious about the dip that may come with it, which often is not as healthy as the vegetables they are served with.
Watch the sodium
Cardiologists are familiar with rising cases of acute heart failures presenting as emergencies at this time of the year. Sodium is the culprit in many of these cases often resulting from dietary indiscretion this time of the year. Surrounded by families and friends with fun times rolling, it is not unusual for patients with weak hearts and heart failure to indulge in meals with high sodium content. This is often compounded by poor compliance with medications at this time of the year.
Limiting sodium intake is very critical but can be quite challenging this time of year. Excess sodium in your bloodstream results in increased water retention in your blood vessels, leading to a rise in blood pressure or hypertension. While many individuals tend to focus on table salt, the reality is that most sodium in the typical urban diet is derived from processed foods. Anything that is canned or processed (and this includes different types of hams) is likely very rich in sodium and should be avoided especially by individuals with known medical history of high blood pressure or heart failure.
Dietary guidelines in the US recommend that adults consume no more than 2,300 milligrams of sodium a day while the American Heart Association recommends an ideal maximum of 1,500 milligrams a day for most adults. The body has an incredible ability to adapt and so the less salt you use, the less salt you would crave for resulting in an overall healthier you. Keep this in mind while you enjoy the holidays.
Do not drink to be merry
Alcohol is a culprit in raising blood pressure and can also lead to fluid overload in individuals with weak hearts or heart failure. Heavy alcohol intake can raise your blood pressure. In most countries, dietary guidelines allow for moderate drinking (two drinks or less in a day for men, and one or less for women), but paying attention to what's in your holiday cocktail is a wise idea. Not all cocktails are created equally. Margaritas, for example, are served in salt-rimmed glasses. Watch those.
Lower your stress level
The holidays can be fun but for some people, it brings a lot of stress. The pressure to achieve a perfect holiday can lead to unwarranted pressure. Stress-related hormones have been linked to increased risk for depression, diabetes, and high blood pressure. Increased stress is also associated with immuno-suppression and increased susceptibility to several illnesses. Stress can also lead to excess alcohol intake, overeating and drug use which can all be detrimental to your health. It's important to dial down the pressure to control your stress level and increase your chill factor. Consider massage therapy, yoga, long walks, visits to nature parks or art shows or simply rest.
What about medications?
While over-the-counter medications are generally safe, there are some pointers that are worth noting. Many commonly used decongestants can elevate your blood pressure. Be sure to look at the warning labels and when in doubt, speak to your doctor or health-care provider for guidance.
As previously noted, compliance with routine medications may pose a problem to some individuals at this time of the year. We recommend proactive efforts to set reminders and trackers to assist you in remembering to take your medications. This can keep you away from an unplanned trip to the hospital emergency room. Now you know some simple measures to take to protect your heart health during this holiday. What if you have a heart-related emergency despite all these precautions.
Your health insurance card is neither your credit card nor debit card
Many individuals with health insurance are under the false impression that they are covered in cases of heart-related emergencies. This is far from reality. In almost all cases, insurance pre-authorisation cannot be obtained in a timely manner when emergency situations require immediate intervention as in heart attack cases. In most instances, your insurance company may insist on a five–seven day window for pre-authorisation which may be detrimental to your care if this is your only source of financing for care and most likely, they would be unavailable to respond during the holiday period. In these situations, unless there is an alternative way of financing emergency treatment, care may be unduly delayed with potentially adverse consequences. It is advisable therefore to have contingency plans for emergency situations irrespective of your health insurance coverage. This is particularly important for family members and friends visiting from overseas as the health system in Jamaica is structured differently from those in the USA and UK ,for example, when it comes to emergency care services.
What to do in heart-related emergencies
Forward planning is always an advantage in dealing with heart related emergencies especially for those individuals with prior history or higher risk for heart disease. It is wise to have a good understanding of the resources available for emergency heart care in your area including knowing which ambulance services are available and how to access them and most importantly knowing which hospitals have the required infrastructure and medical personnel to handle emergency heart conditions. The telephone number and address of these services and facilities should be readily accessible to everyone in the household.
If all fails, DO NOT PANIC. The heart team at the Heart Institute of the Caribbean Heart Hospital is open 24/7 during the holiday period with medical officers on duty at the hospital 24/7, and we have waived emergency room doctors charges until December 31, 2022, to ensure that our citizens are better protected and can enjoy their holidays without worry. This is our Christmas gift to Jamaicans. The call number is 876-906-2106.
HIC Heart Hospital Emergency Room is open for all heart-related emergencies, 24/7 during this holiday period. Merry Christmas and stay safe.
Dr Ernest Madu, MD, FACC and Dr Paul Edwards, MD, FACC are consultant cardiologists for Heart Institute of the Caribbean (HIC) and HIC Heart Hospital. HIC is the regional centre of excellence for cardiovascular care in the English-speaking Caribbean and has pioneered a transformation in the way cardiovascular care is delivered in the region. HIC Heart Hospital is registered by the Ministry of Health and Wellness and is the only heart hospital in Jamaica. Correspondence to info@caribbeanheart.com or call 876-906-2107
2 years 7 months ago
La Zurza is adapting to living with the danger of contracting cholera
Santo Domingo, DR
The residents of the La Zurza sector, a locality of the National District where four new cases of cholera were confirmed almost a week ago, have had to modify their habits and take extreme hygiene measures to avoid contracting the disease.
Santo Domingo, DR
The residents of the La Zurza sector, a locality of the National District where four new cases of cholera were confirmed almost a week ago, have had to modify their habits and take extreme hygiene measures to avoid contracting the disease.
Housewives, the elderly, and young people said they only use water from the water tanks recently installed by the Santo Domingo Aqueduct and Sewerage Corporation (CAASD) for cooking and doing their chores.
“At every certain point, there are four large water tanks that are filled twice a day and with that water we do everything, because we cannot use water from the well or from the river, due to the weeds,” said Mariela Veras, referring to the degree of contamination of the La Isabela River.
Although the Dominicans said they were aware of the threat posed by cholera, the Haitians residing in the area continue to bathe and even wash their clothes in the pool, which shows how unhealthy it is.
Given this situation and the number of Haitians residing in the area, the health authorities have prepared awareness material in Creole and Spanish so that foreigners can receive in their own language the necessary preventive information to avoid the spread of the dangerous disease.
“We have been educating them house by house, we are taking them educational material in Spanish and Creole because there are some foreign citizens here, but the Dominicans have mostly heeded the call for prevention, which is what we are looking for,” said the director of Area IV of Public Health, Jesús Surdí.
On the other hand, during a tour made by journalists of this newspaper, a brigade of workers of the Mayor’s Office of the National District was observed in the area, which has been cleaning all the places that could be a focus of bacteria since yesterday morning.
Mobile hospital
By order of the Minister of Public Health, Daniel Rivera, a mobile hospital was installed last Monday in La Zurza. A team of doctors assists all citizens who present any symptomatology related to cholera.
Fewer patients
Dr. Máximo Canela, in charge of the unit, explained to journalists of Listín Diario that, although the number of patients has gradually decreased, each patient is evaluated, submitted to treatment, or referred to a hospital center, depending on the case.
He added that they are also doing “an educational work by handing out flyers containing essential information on cholera.”
A week ago, the Ministry of Public Health confirmed four new cases of cholera, for a total of six in the country. All correspond to Dominican citizens residing in the La Zurza sector of the National District.
The health authorities urged the population not to be alarmed, to remain alert to reports, and to follow prevention measures such as frequent hand washing, washing food properly, eating well-cooked food, and drinking only potable water.
They also recommend going to the nearest health center for investigation and timely treatment if you have any diarrheal events.
The Ozama cordon
On Thursday, the proposal of the Listin Diario newspaper in its Wednesday editorial to cordon off and prohibit the access of bathers to the Isabela and Ozama rivers due to their high levels of contamination and the recent incidence of cholera bacteria was positively accepted by the Ministry of Health.
According to Dr. Daniel Rivera, Minister of Health, the analyses to understand whether or not it is necessary to limit the passage to both river sources are already underway.
Rivera added that, as Public Health, they are going to wait until they see the cultural studies in the waters of the two rivers to proceed to accompany the acting institutions as much as they have done in the intervention process developed by the Ministry in the capital sector of La Zurza, where the first cases of cholera have appeared in the country.
KEYS
Cases and tests
The Ministry of Public Health reported that eight cases had been confirmed in the Dominican Republic, and six others are awaiting results. It explains that since the cholera cases appeared in Haiti, more than 3,000 tests have been carried out in the country to detect the disease.
Prevention
To combat the disease, the authorities continue to intensify preventive measures through water chlorination, monitoring in schools where toilets and pipes are being repaired, installing new water tanks, creating wells for drinking water supply, and cleaning rivers.
2 years 7 months ago
Health, Local