Health Archives - Barbados Today
Lack of early autism screening a major concern, says association head
3 months 1 week ago
Health, Local News
Research alert: High cannabis use linked to increased mortality in colon cancer patients - EurekAlert!
- Research alert: High cannabis use linked to increased mortality in colon cancer patients EurekAlert!
- Colon cancer patients are 24 times more likely to die within 5 years if they had this habit before their diagnosis New York Post
- High Cannabis Use Linked to Increased Mortality in Colon Cancer Patients UC San Diego Today
- Dirty habit millions admit to daily linked to 20x higher colon cancer death rate, says shock study Daily Mail
3 months 1 week ago
Medical News, Health News Latest, Medical News Today - Medical Dialogues |
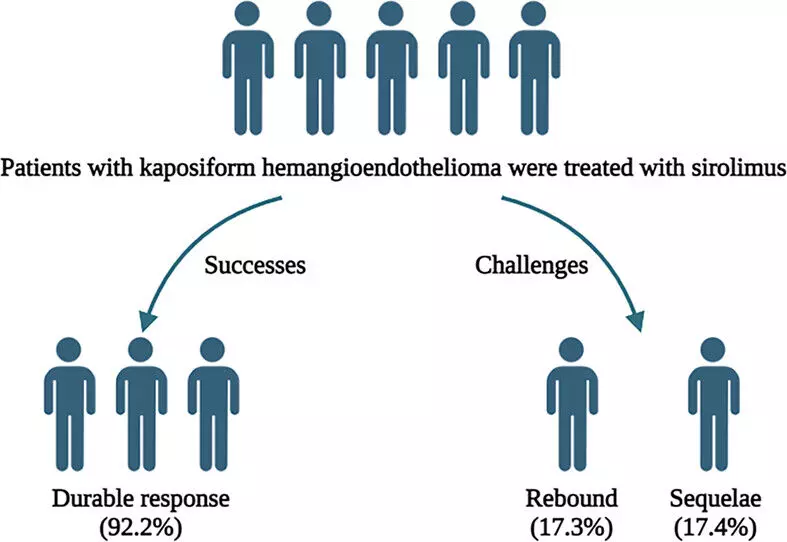
Low-Dose Sirolimus as Effective as High-Dose for Kaposiform Hemangioendothelioma Treatment, suggests study
3 months 1 week ago
Dermatology,Dermatology News,Top Medical News
PM on first official visit to Bolivarian Republic of Venezuela
3 months 1 week ago
Agriculture/Fisheries, Business, Health, Politics, PRESS RELEASE, Travel/Tourism, andy williams, bolivarian republic of venezuela, dickon mitchell, joseph andall, venezuela. nicolas maduro moros
When Hospitals Ditch Medicare Advantage Plans, Thousands of Members Get To Leave, Too
3 months 1 week ago
Aging, Health Care Costs, Health Industry, Insurance, Medicare, Rural Health, CMS, Connecticut, Delaware, Hospitals, Maine, Massachusetts, Medicare Advantage, Michigan, Minnesota, Nebraska, New York, South Dakota, texas
Cuando los abuelos ya no te reconocen
3 months 1 week ago
Aging, Mental Health, Noticias En Español, Dementia, Latinos, Maine, Maryland, Washington
Opinion: Therapy and poetry have more in common than you think
3 months 1 week ago
First Opinion, Mental Health
New study shows most office coffee machines contain cholesterol-raising substances - Surrey Live
- New study shows most office coffee machines contain cholesterol-raising substances Surrey Live
- Filter, cafetière or Aeropress: The healthiest way to brew coffee The Telegraph
- Cholesterol-raising substances could be in most office coffee machines The Mirror US
3 months 1 week ago
Health – Demerara Waves Online News- Guyana
Region Nine gets high marks for HPV vaccination says health minister at Project HealthBridge launch
3 months 1 week ago
Health, News, cervical cancer, HPV vaccination, launch, Project HealthBridge, Rotaract Club of the University of Guyana (RCUG)
Health – Demerara Waves Online News- Guyana
More US forensic pathologists expected for Adriana Younge’s postmortem
3 months 1 week ago
Crime, Health, News, Politics, Adriana Younge, autopsy, forensic pathologists, Gary L Collins, Glenn A Rudner, postmortem, Shubhakar Karra Paul, transparency
Fox News AI Newsletter: Woman says ChatGPT saved her life - Fox News
- Fox News AI Newsletter: Woman says ChatGPT saved her life Fox News
- Woman says ChatGPT saved her life by helping detect cancer, which doctors missed Fox News
- ChatGPT Diagnosed a Woman with Blood Cancer a Year Before Her Doctors Found It People.com
- AI chatbot saves woman's life by diagnosing cancer after doctors dismissed her symptoms Deccan Herald
- My blood test results were normal - but two subtle symptoms led to deadly cancer diagnosis Daily Mail
3 months 1 week ago
Study Confirms The 3 Habits That Age Your Brain Faster - MindBodyGreen
- Study Confirms The 3 Habits That Age Your Brain Faster MindBodyGreen
- I'm a neurologist—don't do these 3 things I regret doing when I was young CNBC
- Without Awareness, These Habits Can Slowly Damage The Brain VOI.ID
- Dementia warning as four habits identified as worst for cognitive decline Daily Record
- 3 Brain-Damaging Habits to Avoid in Youth, According to Neurologists وطن. يغرد خارج السرب
3 months 1 week ago
Walking for less than an hour, thrice a week can have this profound impact on brain - Times of India
- Walking for less than an hour, thrice a week can have this profound impact on brain Times of India
- Exercise boosts brain health — even when energy is low Show Me Mizzou
- Even Light Exercise Could Help Slow Cognitive Decline in People at Risk of Alzheimer’s UC San Diego Today
- New Research Reveals the Secret to Beating Brain Fog in Retirement SciTechDaily
- Even Low-Intensity Exercise May Help Prevent Alzheimer’s Everyday Health
3 months 1 week ago
Medical News, Health News Latest, Medical News Today - Medical Dialogues |
Abbvie seeks USFDA nod for trenibotulinumtoxinE for glabellar lines treatment
3 months 2 weeks ago
News,Industry,Pharma News,Latest Industry News