The Host
Julie Rovner
KFF Health News
@jrovner
Read Julie's stories.
Julie Rovner is chief Washington correspondent and host of KFF Health News’ weekly health policy news podcast, “What the Health?” A noted expert on health policy issues, Julie is the author of the critically praised reference book “Health Care Politics and Policy A to Z,” now in its third edition.
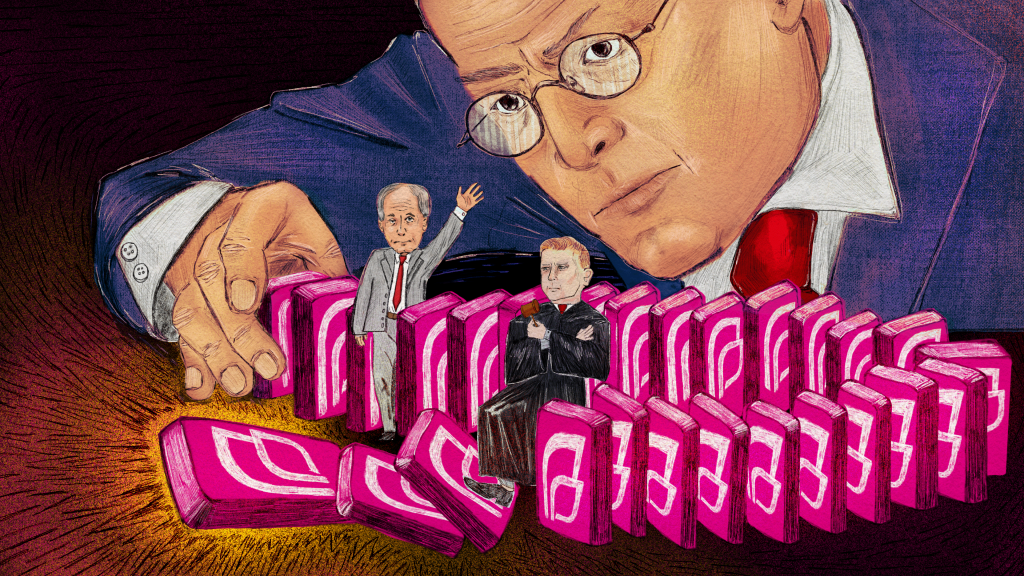
On September 2, 1974, President Gerald Ford signed into law the Employee Retirement Income Security Act, better known as ERISA. While the law was primarily intended to regulate and protect worker pensions, it also fundamentally changed how health insurance is provided and regulated in the United States. Fifty years on, ERISA plays a role in nearly every detail of health insurance and has had a profound impact on the entire health care sector.
To note this anniversary, in this week’s special episode of KFF Health News’ “What the Health?”, host and KFF Health News chief Washington correspondent Julie Rovner discusses the law’s past, present, and future with three experts on ERISA: Larry Levitt of KFF, a health information nonprofit that includes KFF Health News; Paul Fronstin of the Employee Benefit Research Institute, a nonprofit; and Ilyse Schuman of the American Benefits Council, a trade group advocating for employers that sponsor worker benefit plans.
click to open the transcript
Transcript: Happy 50th, ERISA
KFF Health News’ ‘What the Health?’ Episode Title: ‘Happy 50th, ERISA’ Episode Number: 360Published: Thursday, Aug. 15, 2024
[Editor’s note: This transcript was generated using both transcription software and a human’s light touch. It has been edited for style and clarity.]
Julie Rovner: Hello, and welcome back to “What the Health?” I’m Julie Rovner, chief Washington correspondent for KFF Health News. Usually, I’m joined by some of the best and smartest health reporters in Washington, but today, we have a special episode for you. We’re taping this week on Monday, Aug. 12th, at 2 p.m. As always, news happens fast, and things might’ve changed by the time you hear this — although this time, I hope not. So here we go.
So if you follow health policy, you’re likely familiar with the big federal laws that have shaped how health care in the U.S. is organized and delivered and paid for. Medicare and Medicaid in 1965, HIPAA in 1996, and the Affordable Care Act in 2010, just to name a few.
One you may not have heard as much about is ERISA, the Employee Retirement Income Security Act, which was signed in 1974 by then-President Gerald Ford. This fall marks 50 years since ERISA became law. ERISA, as its name suggests, is mostly about protecting pension benefits for workers. It was inspired, at least in part, by the collapse of a pension fund when a plant that built Studebaker cars in Ohio shut down in 1963. But, at least as legend has it, at the very last minute in the House-Senate Conference in 1974, someone decided to add health benefits to ERISA’s scope, and that literally changed the entirety of how health benefits are regulated in the U.S.
I am pleased to have an all-star panel here to join us to talk about what ERISA has meant to health policy and what it’s likely to mean going forward as it begins its second half-century. Larry Levitt is executive vice president for policy here at KFF and one of only a few people in the organization even nerdier than I am about things like ERISA. Paul Fronstin is director of health benefits research at the Employee Benefit Research Institute, a nonpartisan think tank that does research and education. Paul has also taught me more about ERISA over the years than probably any other single person.
Finally, Ilyse Schuman is senior vice president of the American Benefits Council, which represents large employers and other providers of health and retirement benefits through employer-sponsored plans. Ilyse also spent several years on Capitol Hill working on the Senate committee that oversees ERISA policy. So, a lot of knowledge here in our podcast box. Thanks for all of you for being here.
Ilyse Schuman: Thank you
Larry Levitt: Great to be here.
Rovner: So let’s start at the beginning. How did health benefits wind up being covered in a law that was aimed at retiree pensions?
Paul Fronstin: None of us were here or there at the time, so I think anything we know is second- or third-hand information. And like you said, the provision was inserted at the last minute, but I think there were a lot of conversations about it leading up to it being inserted at the last minute. I think a lot of it had to do with some tensions between state regulation and federal regulation, because there were self-insured health plans in existence and self-insured benefits more generally in existence before ERISA passed.
And clearly those plans wanted some federal protection regarding what they were doing, and the states wanted more regulation. And I’ve read a little bit about this over the years, and there was certainly some lobbying for and against having a provision in there to protect self-insured plans from state regulation. So the conversations were happening. It just … the language probably just didn’t make it into the legislation till the last minute.
Schuman: And I think certainly the landscape back in 1974, as Paul talked about, was that more and more states were creating, with respect to health care, their own versions of various laws. And so self-funded plans, large employers like our members — a number of them were back in existence 50 years ago, some weren’t — were finding it increasingly difficult to be able to administer their self-funded plans on a uniform basis nationwide.
So it wasn’t in the backrooms when they were actually drafting the legislation, but certainly note that the nationwide landscape in this growing patchwork of state health laws was becoming increasingly problematical for self-funded health plans.
Levitt: Yeah. I mean, this was also a period when health insurance was changing quite dramatically. I mean, before this time health insurance was pretty simple. It was called indemnity insurance, right.
You went to the doctor, you went to the hospital, you got a claim, you filed it with your insurance company, and they paid 80% of it. This was a time when PPOs [preferred provider organizations] were starting, managed care, HMOs were really just getting their start. So there was a need for much more regulation because insurance was getting more complicated.
Fronstin: Yeah. To some degree, the HMO Act of, what, 1973, right, just the year before. So HMOs were just coming on the scene, and that may have played into this as well.
Rovner: So back in 1945, when really none of us were in the room, Congress passed something called the McCarran-Ferguson Act, which was supposed to ensure that states rather than the federal government retained the authority to regulate insurance. What happened in ERISA to change that? Ilyse, I think you were already sort of referring to this. And what do we mean when we talk about ERISA preemption? That’s a phrase that people hear a lot and their eyes glaze over.
Schuman: Sure. Well, their eyes may glaze over but it really is foundational to millions of Americans and their families that are covered by employers who decide that they want to self-fund their plans. That means that they’re the ones that decide that, “Hey, we’re going to take the risk as offering these benefits instead of the carrier.”
Rovner: So they’re not actually buying insurance because …
Schuman: That’s …
Rovner: … they’re paying the bills.
Schuman: They’re doing more than just paying the bill. They’re the ones that are ultimately assuming the risks of those claims, too. And I think the value. So maybe — just to step back before we talk about what a preemption is — is what we talk about employers who decide to self-fund versus those that don’t. Admittedly, many of those that self-fund are larger employers, but again, they say that “We will take the risk of paying for the claims of our health insurance coverage instead of the carrier. But along with that, we get the flexibility and we get the ability to design and implement health coverage that we think meets the needs of our population. That’s enabled us to” — speaking again from self-funded employers — “to implement innovative designs with the assurances that they could implement those, they could administer that on a uniform basis nationwide.” So that’s really what we’re talking about. Preemption is the ability of self-funded employers to administer those benefits on a uniform basis nationwide.
And yes, getting back to McCarran-Ferguson, and if you want to talk through the sort of various layers of ERISA preemption, is there’s something called the savings clause, which is OK. So ERISA says: “First threshold level, we are going to preempt state laws.” But there’s a savings provision that says basically: “If you’re in the business of insurance, states can regulate that.” But then there’s this deemer clause — this is really nerdy now, so some of your audience may be wondering here what we’re talking about …
Rovner: I remember learning this many, many years ago.
Schuman: No. Yeah. So if you’re in law school, take note that the deemer clause means that self-funded group health plan is deemed not to be in the business of insurance; meaning that they don’t have to comply with those state insurance laws.
Levitt: And here’s where this gets really tangible for people, right? So 150 million people have insurance coverage through an employer. It’s the biggest source of health coverage. But 65% of them are in self-insured plans, like Ilyse was talking about. And those self-insured plans are exempt from state regulation.
So if a state is regulating insurance, let’s say mandating benefits, mandating coverage of IVF, mandating coverage of preventive care, mastectomies, whatever — those regulations that states are putting in place do not apply to most people with employer-sponsored insurance because they are in these self-funded plans.
Rovner: And, of course, the continuing complications that a lot of people who are in these self-funded plans don’t know it because they have an insurance card and it says Blue Cross or Aetna or whatever, because, in their case, they have an insurance card, but the insurer is not providing insurance, right?
Levitt: No, it’s remarkable. We did a survey of consumers about their experiences with health insurance. And we asked them, “What government agency do you think you would turn to with a problem with your insurance?” And literally zero people said the Department of Labor, which is the government agency that actually enforces ERISA.
Rovner: But I guess what I was asking about are third-party administrators, which I think most people have never heard of until they discover that they’re not subject to their state’s requirement.
Levitt: Absolutely. I mean, it gets really confusing, right? Because it might be that UnitedHealthcare is administering this self-funded plan, but you, as an employee in this plan, have no way of really understanding is that a self-insured plan administered by UnitedHealthcare? Or is that an insurance plan administered by UnitedHealthcare? And then there are these third-party administrators that you’ve never even heard of that are administering them for many employers.
Rovner: Paul, you wanted to add something.
Fronstin: We need to distinguish between ERISA and self-insured plans, right, because they’re not one and the same. ERISA also covers fully insured plans.
Schuman: Right.
Fronstin: So fully insured plans are regulated both by ERISA and at the state level. And then you’ve got some self-insured plans like government plans that are not covered by ERISA, right? But they’re self-insured. So it’s even more complicated than what we’re making it out to be when we talk about ERISA, preemption, and self-insurance. That’s just one aspect of ERISA.
Schuman: And I think to the point about employees not sure what covers them, what doesn’t cover them. Again, for self-funded large employers, I mean, I think most of the employees understand from their employer, from the group health plan, what the terms of the plan are, and what the benefits are. And I think in some ways, perhaps less complex than, OK, if you’re an employee working in Kentucky, you have one plan. If you’re an employee working in New York, you have another plan. And employees talking to each other and saying, “Hey, how come you have that and I don’t have this?”
So I think that the clarity or the consistency is important not just for employers who are administering the plan, but for employees understanding what the terms of the plans are. And also, two things about sort of the benefits and what’s covered. There’s a difference between a state saying, “OK, you have to cover this benefit and have to cover it in precisely this way” versus employers who say, “Look, it’s really important for our population, to be healthy and productive, to have these benefits, and so we’re going to offer this benefit. We’re just going to do it in the same way nationwide.”
And remember, ERISA, if the federal government, as it has done over the past, wants to make changes to … that are applicable to group health plans, it can amend and has amended ERISA to do that. So the market reforms, for example, in the Affordable Care Act, were applicable, and the Public Health Service Act, were sort of incorporated into ERISA. The Genetic Information Nondiscrimination Act, for example, amended ERISA. So it’s like that’s the lever to make changes to ERISA that will be applicable to self-funded plans as well is at the federal level.
Rovner: When I was first covering Congress in the 19… late-1980s and early-1990s, you didn’t go there. If you wanted to do something about health policy, you didn’t touch ERISA. I think lawmakers were afraid of reopening it and getting into all kinds of fights. Why did that finally change?
Levitt: I mean, I think there was a growing recognition, particularly with the Affordable Care Act, that there were just some minimum thresholds that health coverage had to meet to be legitimate coverage. So if you look at what the ACA did, and as Ilyse said, those applied to all employers, all group health plans through the amendments to ERISA.
And these were things like no preexisting condition exclusions, coverage of preventive services with no patient cost sharing, no annual on lifetime limits, a cap on out-of-pocket costs. And probably the most popular provision of the ACA, coverage of dependents up to age 26. There was no way to reach everyone with insurance without amending ERISA under the Affordable Care Act.
Fronstin: Yeah. But there were examples, pre-ACA, that affected all plans, or most plans, like mental health parity we didn’t mention. Well, there’s been a couple of instances of that. And certainly the Clinton health plan tried this and didn’t succeed in the early 1990s.
Rovner: And HIPAA …
Levitt: I mean …
Rovner: … which was, I guess, the first major walk into ERISA since ERISA had been passed.
Levitt: Right. Or even COBRA. The ability to continue your insurance after you leave an employer was an amendment to ERISA.
Rovner: That’s right. And that was in 1986.
Fronstin: Yeah, and even that could be confusing because it exempts smaller employers, right. But you got the mini-COBRA laws at state level that affect some of those employers, but not every state has one.
Rovner: Yeah. And Paul, you were referring to this. We should probably talk about who’s not subject to ERISA because I don’t think anybody mentioned church plans. There’s a rule, and then there’s all these exceptions.
Fronstin: I think the two major categories are church plans, and I’m not sure we even have a good handle on how many people are covered by church plans because a lot of them tend to be small businesses, and they may not even offer coverage. And federal, state, and local government. I’m not sure if there’s another category in there that’s not covered by ERISA. I believe that the state and local governments have their own law that’s similar to ERISA, but it’s not ERISA.
Schuman: And I think when we talk about covered by ERISA, certainly it’s, What does ERISA afford? It’s not just about self-funded employers being able to offer uniform benefits nationwide. There are important protections. There are important disclosure requirements for employees, for participants that are included in there that are applicable to all ERISA plans, self-funded and insured plans, and obviously on the retirement plans, too.
But I just think it’s really important that we look to see the idea behind ERISA was that, yes, there will be this uniformity for self-funded plans. But for all ERISA plans, there are these protections and safeguards in there that are embedded in the law for the benefit of participants.
Rovner: And that’s why you used to get a phone-book-thick, “This is your plan documentation.” Now, it’s all online, and it’s all in 4-point type. But that’s where that comes from, right? At the requirement that you be told everything that your plan covers.
Schuman: Right. Correct.
Rovner: So, Larry, you kind of referred to this earlier. Self-funded ERISA plans are regulated not by the states but by the Department of Labor, which most people don’t know. And for a long time, if you were injured or someone died as a result of being denied care, the only thing that they could recover was the cost of the care that was denied. Not any damages for what happened. When did that finally change? And has it finally changed? What do you do now if you’re injured — you can’t go to your state regulatory agency?
Levitt: No, there have been some changes to that, but enforcement of ERISA is still relatively light at the administrative level compared to what state insurance departments do. And the Department of Labor just seems very far away to people compared to a state insurance department.
I think it’s really this structure of ERISA that, Julie, you said people were always resistant to amending in Congress, that has been resistant to amendment, right? I mean, this idea that states regulate insurance directly but that states cannot regulate group health plans under ERISA. And that’s had far-reaching health policy implications. So states looking to do employer mandates or anything that directly affects those group health plans, employer health plans, and that’s maybe …
Rovner: Also, states looking to do single-payer plans, right?
Levitt: Yeah. No, I mean, single-payer there might be some ways around ERISA through single-payer and taxation, but ERISA has been a barrier to state health reform efforts, for better or for worse.
Schuman: If maybe we can just step back 50 years, I think it’s … I wrote down this quote from one of the authors of ERISA, specifically on the ERISA preemption, and that was by Rep. John Dent, who was a Democrat from Pennsylvania who identified the ERISA preemption as the law’s crowning achievement.
And he said it was the crowning achievement because, without it, the legislation would not have enjoyed the support of both labor and management since it’s so fundamental for the ability of multistate employers to sponsor benefit plans to workers nationwide. So I think just kind of getting back into the minds of the drafters of ERISA, that bargain, if you will, that became ERISA preemption was really foundational to the law passing.
Rovner: And you could see why it would make sense. If you work for a national company and you get transferred from one state to another, your insurance shouldn’t change dramatically.
Schuman: Yeah. And I think fast-forward 50 years, and we’ve got, certainly, post-pandemic or after the pandemic, an increasingly mobile and remote workforce. And we have heard repeatedly about how ERISA preemption really promotes that worker mobility and the ability to work out of your house in another state or to be able to transfer from one location to another.
So think a little bit if we just see how the workforce itself has evolved, I think that ERISA preemption provision may become even more important. And I think increasingly, it’s not just large employers that find themselves — like nationwide or multistate employers — but because the workforce is more remote and mobile, and wants to be, that more and more employers of multistate employers, too.
Levitt: I would say we have increasingly seen smaller employers self-funding, and there are some advantages to that, right? They don’t necessarily have to pay premium taxes to states, and they are exempt from state benefit mandates that apply over and above beyond the Affordable Care Act. I mean, insurers have come up with very creative ways of allowing smaller businesses to self-fund and avoiding some of the risk by layering lots of reinsurance on top of that.
Fronstin: I was going to say, along with self-funding comes ease of administration here. Ilyse, you call it uniformity of benefits. But I think of employers, they don’t want to be offering 50 different health plans in 50 different states. And to the degree you’ve got the states doing something — whether it’s a single-payer or something short of that — employers, they just want to offer everyone the same benefit and make it as easy as possible to do so.
And my concern is if they had to comply with 50 different state laws to do so or create 50 different benefit plans, especially today with the ACA guaranteed issue and subsidized coverage, you’ll get to the point where if employers didn’t have the ability to provide one benefit plan across all 50 states, they’re not going to do it anymore, right? They’ve got … pre-ACA might’ve been different, but now they’ve got an alternative where their employees could get coverage if they didn’t offer coverage themselves.
Rovner: So that was all predicted. This huge movement away from employer-provided coverage after the ACA passed was predicted, and it didn’t happen.
Fronstin: I was one of those people predicting it. Yeah. Before the ACA passed, I was one of those people predicting it. And I think what happened is: One, being employers, they still value the benefit. They still understand there are business reasons to offer it, and they haven’t had a good excuse to get rid of it.
We haven’t had — other than the recession tied to covid — we haven’t had a recession. Our unemployment rate has been at historically low rates. And I think employers, they don’t want to mess with something that’s working for the most part because they use it to recruit and retain employees for the same thing they were doing back in the 1940s and ’50s when they first started offering it.
Schuman: I think it’s important to delineate the employer voice in here. And I think maybe there’s a perception that employers are just writing the checks or employers and health plans are kind of conflated. But employers are doing a lot more than just writing a check. And I think those, again, that have decided to self-fund want to be able to have control over how they’re spending their health care dollars. So again, they can try to drive more affordable, higher-value, higher-quality health care.
And so it’s not just about who writes the check, but the reasons behind employers saying, “Hey, we’re going to be spending … we spend a whole lot of money on our health benefits because we recognize that it’s good business. It’s good for employees. But we want to be able to have the ability to try to drive improvements in that to drive higher-value care.” And so that’s enabled by ERISA. So the health reforms and the health innovation, certainly there’s a lot coming from the states, but there’s a lot coming from employers, too.
Rovner: So what are the big issues going forward for ERISA? I mean, obviously, there’s still, if you Google ERISA, you get all kinds of lawsuits and challenges. And I mean, it’s still a very lively part of the law 50 years on.
Levitt: I mean, I think, Julie, you mentioned these lawsuits, and that is potentially a big issue going forward. Something called the Consolidated Appropriations Act added some transparency in fees that self-insured employer plans paid to providers. And that’s opened the door to some lawsuits challenging whether group health plans, ERISA plans, are acting as appropriate fiduciaries in trying to get the lowest costs, particularly for prescription drugs. And these started out as kind of a fringe movement, but I think pose some potential risks for group health plans.
Rovner: Ilyse, what are employers most concerned about?
Schuman: Well, I think that employers seeing the growing number of states that are trying to chip away, if not erode in a fundamental way, ERISA preemption is really alarming. A lot of these efforts have come up around pharmacy benefit managers and efforts to regulate pharmacy benefit managers at the state level.
But the way that they’ve done it, the states have really taken direct aim at ERISA preemption and self-funded plans and, I think, has much broader implications for self-funded group health plans beyond just the PBM context. And so I think that they’re looking at the growing number of states that are interested in passing laws that really erode ERISA preemption as very alarming.
Rovner: So I want to go around the table before we end. Sort of what do you think has been the biggest impact on the health system of ERISA, both for good and for not so good? I mean, it’s certainly one of the things that makes it so confusing to understand and explain. Larry, you want to go first?
Levitt: I think the biggest impact of ERISA has been putting the brakes on some state health reform efforts. States have found ways to get around it. Some raise some issues for employers, like Ilyse was saying, but it has really circumscribed what states can do around health reform. That said, ERISA has provided a very stable regulatory environment for employers and likely allowed employer coverage to grow over time in that environment.
Rovner: Paul?
Fronstin: Yeah, I’d say, in addition to that, it’s allowed employers to be innovative. Not every self-insured employer has been innovative, right? And there’s something like a million employers out there with a thousand or more employees. And the smaller of those are not necessarily being innovative, but they’re learning from the largest ones, right? The jumbo employers, who are trying to do different things when it comes to engaging the health system, right? Engaging hospitals and physicians and pharmaceutical managers.
And I think that that … the lessons learned from what they’re doing trickles down to the smaller self-insured employers, and it trickles out to the health insurers that are offering fully insured plans to small employers.
Rovner: Ilyse.
Schuman: I think ERISA has allowed employers to provide value-driven, comprehensive, affordable, higher-quality health coverage to working families across the country — 150 million, 180 million, guess it depends what stats you’re looking at, and that it’s withstood the test of time.
And I think that probably no stressor, like the pandemic, where many wondered what would emerge from that, and with some dents, but also with a lot of silver linings in terms of employers offering benefits to help their employees navigate through the pandemic. And so I think there’s a resiliency to the employer-sponsored system coupled with the innovation that Paul has mentioned.
Rovner: Last question. Yes or no? Is ERISA going to be around in another 50 years? In other words, are we still going to have this system of health coverage? I promise I will not hold you to it. Just best guess. Larry.
Levitt: I say no.
Rovner: Paul.
Fronstin: I answer “don’t know.”
Rovner:: That’s OK. Ilyse.
Schuman: Well, I will say that I just recently got a tortoise for my family that I’ve found will live 50 or 100 years, so beyond me. So will ERISA be around as long as Veggie, the tortoise? I don’t know.
I think that there’s really an important inflection point. And I think if addressing some of the underlying drivers of rising health care costs and consolidation, I think that if those are addressed, I think employer-provided coverage certainly has the ability to withstand the test of time over the next 50 years.
Rovner: Good. Thank you all so much. This has been great.
Schuman: Thanks a lot.
Levitt: Great. Thanks, Julie.
Schuman: Thank your team.
Levitt: Thanks all.
Schuman: Bye-bye.
Fronstin: Take care, everybody.
Levitt: Bye.
Rovner: Bye. OK, that’s our ERISA anniversary show. Big thanks to our guests, Larry Levitt of KFF, Paul Fronstin of EBRI, and Ilyse Schuman of the American Benefits Council. And before we go this week, we’re looking for your help on a project here at KFF Health News. Are you a young adult confused about navigating the exchanges used to pick plans? Have you bought a plan on an ACA exchange and found that it didn’t cover care you needed? Have you married or taken a job just to get insurance? Did you decide to go without coverage?
Whatever your story, KFF Health News and The New York Times want to hear it. Email your experience to Elisabeth Rosenthal — that’s elisabethr with an S, not a Z — @kff.org. As always, if you enjoy the podcast, you can subscribe wherever you get your podcasts. We’d appreciate it if you left us a review; that helps other people find us, too. Special thanks, as usual, to our technical guru, Francis Ying, and our editor, Emmarie Huetteman. As always, you can email us your comments or questions. We’re at whatthehealth, all one word, @kff.org, where you can still find me. I’m @jrovner on X. We’ll be back in your feed next week. Until then, be healthy.
Credits
Francis Ying
Audio producer
Emmarie Huetteman
Editor
To hear all our podcasts, click here.
And subscribe to KFF Health News’ “What the Health?” on Spotify, Apple Podcasts, Pocket Casts, or wherever you listen to podcasts.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).