PAHO: Mental health must be top of political agenda
Report highlights that while mental health conditions have historically represented a significant source of disability and mortality in the Region, this has been further compounded by the COVID-19 pandemic
View the full post PAHO: Mental health must be top of political agenda on NOW Grenada.
2 years 1 month ago
External Link, Health, coronavirus, COVID-19, jarbas barbosa, Mental Health, paho, pan american health organsation
Burnout Threatens Primary Care Workforce and Doctors’ Mental Health
If you or someone you know may be experiencing a mental health crisis, contact the 988 Suicide & Crisis Lifeline by dialing “988,” or the Crisis Text Line by texting “HOME” to 741741.
CHARLESTON, S.C. — Melanie Gray Miller, a 30-year-old physician, wiped away tears as she described the isolation she felt after losing a beloved patient.
If you or someone you know may be experiencing a mental health crisis, contact the 988 Suicide & Crisis Lifeline by dialing “988,” or the Crisis Text Line by texting “HOME” to 741741.
CHARLESTON, S.C. — Melanie Gray Miller, a 30-year-old physician, wiped away tears as she described the isolation she felt after losing a beloved patient.
“It was at the end of a night shift, when it seems like bad things always happen,” said Miller, who is training to become a pediatrician.
The infant had been sick for months in the Medical University of South Carolina’s pediatric intensive care unit and the possibility that he might not improve was obvious, Miller recalled during an April meeting with physicians and hospital administrators. But the suddenness of his death still caught her off guard.
“I have family and friends that I talk to about things,” she said. “But no one truly understands.”
Doctors don’t typically take time to grieve at work. But during that recent meeting, Miller and her colleagues opened up about the insomnia, emotional exhaustion, trauma, and burnout they experienced from their time in the pediatric ICU.
“This is not a normal place,” Grant Goodrich, the hospital system’s director of ethics, said to the group, acknowledging an occupational hazard the industry often downplays. “Most people don’t see kids die.”
The recurring conversation, scheduled for early-career doctors coming off monthlong pediatric ICU rotations, is one way the hospital helps staffers cope with stress, according to Alyssa Rheingold, a licensed clinical psychologist who leads its resiliency program.
“Often the focus is to teach somebody how to do yoga and take a bath,” she said. “That’s not at all what well-being is about.”
Burnout in the health care industry is a widespread problem that long predates the covid-19 pandemic, though the chaos introduced by the coronavirus’s spread made things worse, physicians and psychologists said. Health systems across the country are trying to boost morale and keep clinicians from quitting or retiring early, but the stakes are higher than workforce shortages.
Rates of physician suicide, partly fueled by burnout, have been a concern for decades. And while burnout occurs across medical specialties, some studies have shown that primary care doctors, such as pediatricians and family physicians, may run a higher risk.
“Why go into primary care when you can make twice the money doing something with half the stress?” said Daniel Crummett, a retired primary care doctor who lives in North Carolina. “I don’t know why anyone would go into primary care.”
Doctors say they are fed up with demands imposed by hospital administrators and health insurance companies, and they’re concerned about the notoriously grueling shifts assigned to medical residents during the early years of their careers. A long-standing stigma keeps physicians from prioritizing their own mental health, while their jobs require them to routinely grapple with death, grief, and trauma. The culture of medicine encourages them to simply bear it.
“Resiliency is a cringe word for me,” Miller said. “In medicine, we’re just expected to be resilient 24/7. I don’t love that culture.”
And though the pipeline of physicians entering the profession is strong, the ranks of doctors in the U.S. aren’t growing fast enough to meet future demand, according to the American Medical Association. That’s why burnout exacerbates workforce shortages and, if it continues, may limit the ability of some patients to access even basic care. A 2021 report published by the Association of American Medical Colleges projects the U.S. will be short as many as 48,000 primary care physicians by 2034, a higher number than any other single medical specialty.
A survey published last year by The Physicians Foundation, a nonprofit focused on improving health care, found more than half of the 1,501 responding doctors didn’t have positive feelings about the current or future state of the medical profession. More than 20% said they wanted to retire within a year.
Similarly, in a 2022 AMA survey of 11,000 doctors and other medical professionals, more than half reported feeling burned out and indicated they were experiencing a great deal of stress.
Those numbers appear to be even higher in primary care. Even before the pandemic, 70% of primary care providers and 89% of primary care residents reported feelings of burnout.
“Everyone in health care feels overworked,” said Gregg Coodley, a primary care physician in Portland, Oregon, and author of the 2022 book “Patients in Peril: The Demise of Primary Care in America.”
“I’m not saying there aren’t issues for other specialists, too, but in primary care, it’s the worst problem,” he said.
The high level of student debt most medical school graduates carry, combined with salaries more than four times as high as the average, deter many physicians from quitting medicine midcareer. Even primary care doctors, whose salaries are among the lowest of all medical specialties, are paid significantly more than the average American worker. That’s why, instead of leaving the profession in their 30s or 40s, doctors often stay in their jobs but retire early.
“We go into medicine to help people, to take care of people, to do good in the world,” said Crummett, who retired from the Duke University hospital system in 2020 when he turned 65.
Crummett said he would have enjoyed working until he was 70, if not for the bureaucratic burdens of practicing medicine, including needing to get prior authorization from insurance companies before providing care, navigating cumbersome electronic health record platforms, and logging hours of administrative work outside the exam room.
“I enjoyed seeing patients. I really enjoyed my co-workers,” he said. “The administration was certainly a major factor in burnout.”
Jean Antonucci, a primary care doctor in rural Maine who retired from full-time work at 66, said she, too, would have kept working if not for the hassle of dealing with hospital administrators and insurance companies.
Once, Antonucci said, she had to call an insurance company — by landline and cellphone simultaneously, with one phone on each ear — to get prior authorization to conduct a CT scan, while her patient in need of an appendectomy waited in pain. The hospital wouldn’t conduct the scan without insurance approval.
“It was just infuriating,” said Antonucci, who now practices medicine only one day a week. “I could have kept working. I just got tired.”
Providers’ collective exhaustion is a crisis kept hidden by design, said Whitney Marvin, a pediatrician who works in the pediatric ICU at the Medical University of South Carolina. She said hospital culture implicitly teaches doctors to tamp down their emotions and to “keep moving.”
“I’m not supposed to be weak, and I’m not supposed to cry, and I’m not supposed to have all these emotions, because then maybe I’m not good enough at my job,” said Marvin, describing the way doctors have historically thought about their mental health.
This mentality prevents many doctors from seeking the help they need, which can lead to burnout — and much worse. An estimated 300 physicians die by suicide every year, according to the American Foundation for Suicide Prevention. The problem is particularly pronounced among female physicians, who die by suicide at a significantly higher rate than women in other professions.
A March report from Medscape found, of more than 9,000 doctors surveyed, 9% of male physicians and 11% of female physicians said they have had suicidal thoughts. But the problem isn’t new, the report noted. Elevated rates of suicide among physicians have been documented for 150 years.
“Ironically, it’s happening to a group of people who should have the easiest access to mental health care,” said Gary Price, a Connecticut surgeon and president of The Physicians Foundation.
But the reluctance to seek help isn’t unfounded, said Corey Feist, president of the Dr. Lorna Breen Heroes’ Foundation.
“There’s something known in residency as the ‘silent curriculum,’” Feist said in describing an often-unspoken understanding among doctors that seeking mental health treatment could jeopardize their livelihood.
Feist’s sister-in-law, emergency room physician Lorna Breen, died by suicide during the early months of the pandemic. Breen sought inpatient treatment for mental health once, Feist said, but feared that her medical license could be revoked for doing so.
The foundation works to change laws across the country to prohibit medical boards and hospitals from asking doctors invasive mental health questions on employment or license applications.
“These people need to be taken care of by us, because really, no one’s looking out for them,” Feist said.
In Charleston, psychologists are made available to physicians during group meetings like the one Miller attended, as part of the resiliency program.
But fixing the burnout problem also requires a cultural change, especially among older physicians.
“They had it worse and we know that. But it’s still not good,” Miller said. “Until that changes, we’re just going to continue burning out physicians within the first three years of their career.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
2 years 1 month ago
Health Industry, Mental Health, Doctors, Maine, North Carolina, Primary Care Disrupted, South Carolina
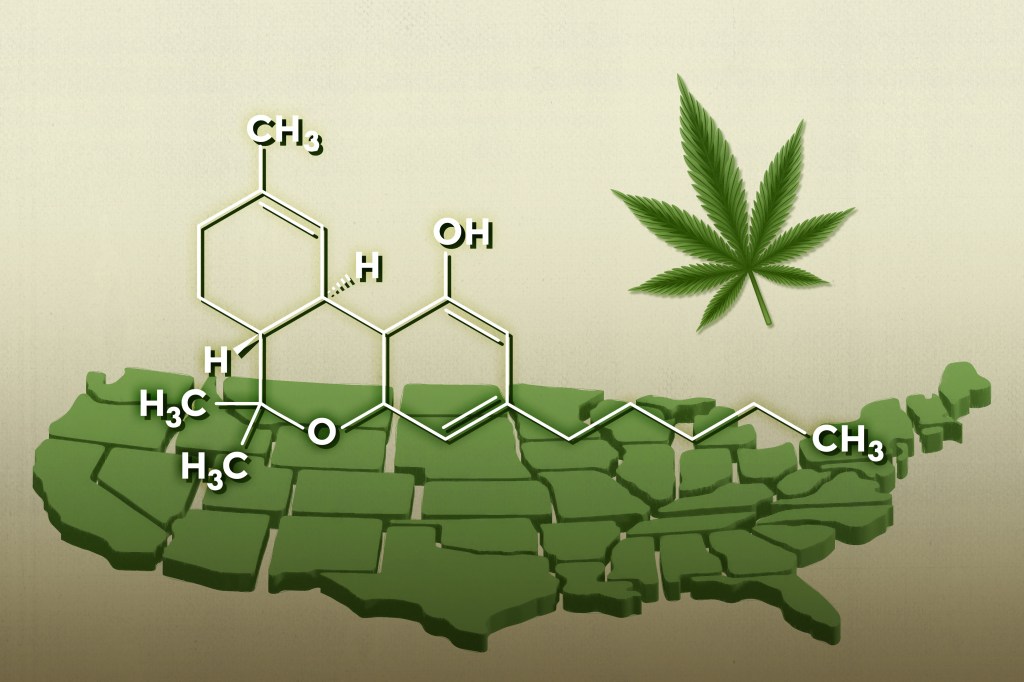
Marihuana legal es más potente que nunca pero no está bien regulada
La marihuana y otros productos que contienen THC, el principal ingrediente psicoactivo de la planta, se han vuelto más potentes y peligrosos a medida que la legalización los ha vuelto más accesibles.
Décadas atrás, el contenido de THC de la hierba solía ser inferior al 1,5%. Hoy, algunos productos tienen más de un 90%.
La marihuana y otros productos que contienen THC, el principal ingrediente psicoactivo de la planta, se han vuelto más potentes y peligrosos a medida que la legalización los ha vuelto más accesibles.
Décadas atrás, el contenido de THC de la hierba solía ser inferior al 1,5%. Hoy, algunos productos tienen más de un 90%.
La euforia de antaño ha dado paso a algo más alarmante. Cientos de miles de personas llegan a salas de emergencias por crisis relacionadas con la marihuana, y millones sufren trastornos psicológicos vinculados al consumo de cannabis, según investigaciones federales.
Pero los organismos reguladores no están a la altura.
En los estados que permiten la venta y el consumo de la marihuana y sus derivados, la protección al consumidor no es consistente.
“En muchos estados, los productos tienen una etiqueta de advertencia y poco más por parte de las entidades reguladoras”, dijo Cassin Coleman, vicepresidente del comité de asesoramiento científico de la Asociación Nacional de la Industria del Cannabis.
En general, el gobierno federal no ha intervenido. Sigue prohibiendo la marihuana como sustancia catalogada en la Lista 1 —como droga sin uso médico aceptado y con un alto riesgo de abuso— en virtud de la Ley de Sustancias Controladas (CSA). Pero en lo que respecta a la venta de cannabis, que muchos estados han legalizado, no regula características como la pureza o la potencia.
La Administración de Drogas y Alimentos (FDA) “básicamente se ha cruzado de brazos y no ha cumplido con su deber de proteger la salud pública”, afirmó Eric Lindblom, de la Facultad de Derecho de la Universidad de Georgetown que anteriormente trabajó en el Centro para Productos del Tabaco de la FDA.
La marihuana se ha transformado profundamente desde que generaciones de estadounidenses la usaron por primera vez.
El cannabis se cultiva para suministrar dosis mucho más altas de THC. En 1980, el contenido de THC de la marihuana confiscada era inferior al 1,5%. Hoy en día, muchas variedades de flores de cannabis —la materia vegetal que se puede fumar en un porro— tienen más de un 30% de THC.
Recientemente, en un dispensario de California el menú incluía una variedad con un 41% de THC.
La legalización también ha abierto la puerta a productos que se extraen de la marihuana pero que no siquiera parecidos: concentrados de THC aceitosos, cerosos o cristalinos que se calientan e inhalan mediante el vapeo o el dab, utilizando dispositivos parecidos a un soplete.
Los concentrados actuales pueden tener más de un 90% de THC. Algunos se anuncian como THC casi puro.
Pocos personifican la expansión de la marihuana de forma tan clara como John Boehner, ex presidente de la Cámara de Representantes de Estados Unidos. El republicano de Ohio se opuso durante mucho tiempo a la marihuana y, en 2011, se declaró “inalterablemente contrario” a su legalización.
Ahora forma parte del consejo directivo de Acreage Holdings, un productor de derivados de la marihuana.
Y Acreage Holdings ilustra la evolución del sector. Su marca Superflux comercializa un producto para vapear —”resina pura en un formato cómodo e instantáneo”— y concentrados como “budder”, “sugar”, “shatter” y “wax”. La empresa anuncia su concentrado de “THCa cristalino” como “lo último en potencia”.
Según el Instituto Nacional sobre el Abuso de Drogas, las concentraciones más elevadas entrañan mayores riesgos. “Los riesgos de dependencia física y adicción aumentan con la exposición a altas concentraciones de THC, y las dosis más altas de THC tienen más probabilidades de producir ansiedad, agitación, paranoia y psicosis”, se explica en su sitio web.
En 2021, 16,3 millones de personas en Estados Unidos —el 5,8% de las personas de 12 años en adelante— habían sufrido un trastorno por consumo de marihuana en el último año, según una encuesta publicada en enero por el Departamento de Salud y Servicios Humanos (HHS).
Esta cifra es muy superior a la suma de los trastornos por consumo de cocaína, heroína, metanfetamina, estimulantes de venta bajo receta, como Adderall, o analgésicos recetados, como fentanilo y OxyContin.
Otras drogas son más peligrosas que la marihuana, y la mayoría de las personas afectadas por su consumo padecieron un caso leve. Pero aproximadamente 1 de cada 7 —más de 2,6 millones de personas— padecieron un caso grave, según la encuesta federal.
La mayoría de los médicos equiparan el término “trastorno grave por consumo de sustancias” con la adicción, señaló Wilson Compton, subdirector del Instituto Nacional sobre el Abuso de Drogas.
El trastorno por consumo de cannabis “puede ser devastador”, afirmó Smita Das, psiquiatra de Stanford y presidenta de un consejo sobre adicciones de la Asociación Americana de Psiquiatría.
Das dijo que ha visto vidas destrozadas por el cannabis: personas de éxito que han perdido familias y trabajos. “Se encuentran en una situación en la que no saben cómo han llegado, porque sólo era un porro, sólo era cannabis, y no se suponía que el cannabis les creara adicción”, explicó Das.
Entre los diagnósticos médicos atribuidos a la marihuana figuran la “dependencia del cannabis con trastorno psicótico con delirios” y el síndrome de hiperémesis cannabinoide, una forma de vómito persistente.
Se estima que unas 800,000 personas realizaron visitas a emergencias relacionadas con la marihuana en 2021, según un estudio del gobierno publicado en diciembre de 2022.
Derecho a desintoxicación.
Un padre de Colorado pensó que era cuestión de tiempo para que el cannabis matara a su hijo.
En la primavera de 2021, el adolescente pasó un semáforo en rojo, chocó contra otro auto —resultando heridos él y el otro conductor— y huyó del lugar, según recordó el padre en una entrevista.
En los restos del accidente, el padre encontró porros, envases vacíos de un concentrado de THC de alta potencia conocido como “wax” y un vaporizador de THC.
En el teléfono móvil de su hijo descubrió mensajes de texto y decenas de referencias al “dabbing” y a la hierba. El adolescente dijo que había estado fumando antes del accidente y que intentó suicidarse.
Semanas después, la policía ordenó su ingreso involuntario en un hospital para una evaluación psiquiátrica. Según un informe policial, creía que lo perseguían francotiradores de un cártel de drogas.
El médico que evaluó al adolescente le diagnosticó “abuso de cannabis”.
“Deja de consumir dabs o wax, ya que pueden volverte extremadamente paranoico”, escribió el médico. “Vete directamente al programa de desintoxicación que elijas”.
Según el relato del padre, en los dos últimos años el adolescente sufrió varias retenciones involuntarias, docenas de encuentros con la policía, repetidos encarcelamientos y una serie de estadías en centros de tratamiento hospitalario.
A veces parecía fuera de la realidad, y enviaba mensajes de texto diciendo que Dios le hablaba y le daba superpoderes.
Los daños también fueron económicos. Los reclamos al seguro médico por su tratamiento ascendieron a casi $600,000 y los gastos de la familia llegaron a casi $40,000 hasta febrero.
En las entrevistas para este artículo, el padre habló bajo condición de anonimato para no perjudicar la recuperación de su hijo.
Está convencido de que la enfermedad mental de su hijo fue el resultado del consumo de drogas. Dijo que los síntomas remitían cuando su hijo dejaba de consumir THC y volvían cuando usaba de nuevo.
Su hijo tiene ahora 20 años, ha dejado la marihuana y le va bien, dijo el padre, y añadió: "No me cabe la menor duda de que el consumo de cannabis fue lo que le causó la psicosis, los delirios y la paranoia".
Regulación estatal desigual
Ahora, el uso médico de la marihuana es legal en 40 estados y el Distrito de Columbia, y el uso recreativo o para adultos es legal en 22 estados más el Distrito de Columbia, según MJBizDaily, una publicación especializada.
Al principio de la pandemia de covid-19, mientras gran parte de Estados Unidos cerró sus negocios, los dispensarios de marihuana siguieron abiertos. Muchos estados los declararon negocios esenciales.
Pero sólo dos estados que permiten el uso para adultos, Vermont y Connecticut, han puesto límites al contenido de THC —30% para la flor de cannabis y 60% para los concentrados de THC— y eximen de los límites a los cartuchos precargados, dijo Gillian Schauer de la Asociación de Reguladores de Cannabis, un grupo de reguladores estatales.
Algunos estados limitan el número de onzas o gramos que los consumidores pueden comprar. Sin embargo, incluso un poco de marihuana puede equivaler a mucho THC, apuntó Rosalie Liccardo Pacula, profesora de políticas de salud, economía y derecho en la Universidad del Sur de California.
Algunos estados sólo permiten el uso médico de productos con bajo contenido de THC; por ejemplo, en Texas, las sustancias que no contienen más de un 0,5% de THC en peso. Y algunos estados exigen etiquetas de advertencia. En Nueva Jersey, los productos de cannabis con más de un 40% de THC deben declarar: "Este es un producto de alta potencia y puede aumentar el riesgo de psicosis".
La normativa sobre marihuana de Colorado tiene más de 500 páginas. Sin embargo, se enfatizan los límites de las protecciones al consumidor: "Este producto se ha producido sin supervisión reglamentaria en materia de salud, seguridad o eficacia".
Determinar las normas adecuadas puede no ser sencillo. Por ejemplo, las etiquetas de advertencia podrían proteger a la industria de la marihuana de su responsabilidad, al igual que hicieron con las empresas tabacaleras durante años. Poner un tope a la potencia podría limitar las opciones de las personas que toman dosis elevadas para aliviar problemas médicos.
En general, en el ámbito estatal, la industria del cannabis ha frenado los esfuerzos reguladores argumentando que unas normas onerosas dificultarían la competencia entre las empresas legítimas y las ilícitas, explicó Pacula.
Pacula y otros investigadores han pedido al gobierno federal que intervenga.
Meses después de terminar su mandato como comisionado de la FDA, Scott Gottlieb hizo un llamamiento similar.
Al quejarse de que los estados habían llegado "muy lejos mientras el gobierno federal permanecía al margen", Gottlieb pidió "un esquema nacional uniforme para el THC que proteja a los consumidores."
Eso fue en 2019 y poco ha cambiado desde entonces.
¿Dónde está la FDA?
La FDA supervisa los alimentos, los medicamentos recetados, los de venta libre y los dispositivos médicos. Regula el tabaco, la nicotina y los vapes de nicotina. Supervisa las etiquetas de advertencia del tabaco. En interés de la salud y la seguridad públicas, también regula los productos botánicos, productos médicos que pueden incluir material vegetal.
Sin embargo, cuando se trata de la marihuana para fumar, los concentrados de THC derivados del cannabis que se vapean o dabean y los comestibles infundidos con THC, la FDA parece estar muy al margen.
La marihuana medicinal que se vende en los dispensarios no está aprobada por la FDA. La agencia no ha avalado su seguridad o eficacia ni ha determinado la dosis adecuada. No inspecciona las instalaciones donde se producen los productos ni evalúa el control de calidad.
La agencia sí invita a los fabricantes a someter los productos del cannabis a ensayos clínicos y a su proceso de aprobación de medicamentos.
El sitio web de la FDA señala que el THC es el ingrediente activo de dos medicamentos aprobados por la FDA para el tratamiento del cáncer. Aparentemente, sólo por eso la sustancia está bajo la jurisdicción de la FDA.
La FDA tiene "todo el poder que necesita para regular de forma mucho más eficaz los productos de cannabis legalizados por los estados", afirmó Lindblom, ex funcionario de la agencia.
Al menos públicamente, la FDA no le ha prestado atención a los concentrados de THC derivados del cannabis o la hierba fumada en porros, sino más bien en otras sustancias: una variante del THC derivada del cáñamo, que el gobierno federal ha legalizado, y un derivado diferente del cannabis llamado cannabidiol o CBD, que se ha comercializado como terapéutico.
"La FDA se ha comprometido a vigilar el mercado, identificar los productos de cannabis que plantean riesgos y actuar, dentro de nuestras competencias, para proteger al público", declaró Courtney Rhodes, vocera de la FDA.
"Muchos, la mayoría de los productos con THC se ajustan a la definición de marihuana, que es una sustancia controlada. La Drug Enforcement Administration (DEA) regula la marihuana en virtud de la Ley de Sustancias Controladas (CSA). Le remitimos a la DEA para preguntas sobre la regulación y aplicación de las disposiciones de la CSA", escribió Rhodes en un correo electrónico.
La DEA, dependiente del Departamento de Justicia, no respondió a las preguntas formuladas para este artículo.
En cuanto al Congreso, quizá su medida más importante haya sido limitar la aplicación de la prohibición federal.
"Hasta ahora, la respuesta federal a las acciones estatales para legalizar la marihuana ha consistido, sobre todo, en permitir que los estados apliquen sus propias leyes sobre la droga", señaló un informe de 2022 del Servicio de Investigación del Congreso.
En octubre, el presidente Joe Biden ordenó al secretario de Salud y Servicios Humanos y al fiscal general que revisaran la postura del gobierno federal respecto a la marihuana: si debería seguir clasificada entre las sustancias más peligrosas y estrictamente controladas.
En diciembre, Biden firmó un proyecto de ley que ampliaba la investigación sobre la marihuana y obligaba a las agencias federales a estudiar sus efectos. La ley dice que las agencias tienen un año para publicar sus conclusiones.
Algunos defensores de la marihuana dicen que el gobierno federal podría desempeñar un papel más constructivo.
"La NORML no opina que el cannabis sea inocuo, sino que la mejor forma de mitigar sus riesgos potenciales es mediante la legalización, la regulación y la educación pública", afirmó Paul Armentano, subdirector del grupo antes conocido como Organización Nacional para la Reforma de las Leyes sobre la Marihuana (NORML).
"Los productos tienen que someterse a pruebas de pureza y potencia", añadió, y "el gobierno federal podría ejercer cierta supervisión en la concesión de licencias a los laboratorios que prueban esos productos".
Mientras tanto, según Coleman, asesor de la Asociación Nacional de la Industria del Cannabis, los estados se quedan "teniendo que actuar como si fueran USDA + FDA + DEA, todo al mismo tiempo".
¿Y dónde deja eso a los consumidores? Algunos, como Wendy E., jubilada en sus 60 años, luchan contra los efectos de la marihuana.
Wendy, que habló con la condición de que no se revelara su nombre, empezó a fumar marihuana en la secundaria en los años 70 y la convirtió en su estilo de vida durante décadas.
Luego, cuando su estado la legalizó, la compró en dispensarios "y enseguida me di cuenta de que la potencia era mucho mayor que la que yo había consumido tradicionalmente", contó. "Parecía haber aumentado de manera exponencial".
En 2020, explicó, la marihuana legal —mucho más fuerte que la hierba ilícita de su juventud— la llevó a obsesionarse con el suicidio.
Antes, la mujer que se define como "hippie de la madre tierra" encontraba camaradería pasando un porro con sus amigos. Ahora asiste a reuniones de Marihuana Anónimos, con otras personas que se recuperan de esta adicción.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
2 years 2 months ago
Health Industry, Mental Health, Noticias En Español, Colorado, Connecticut, FDA, Latinos, Legislation, marijuana, New Jersey, Substance Misuse, texas, Vermont
Health Programs Are at Risk as Debt Ceiling Cave-In Looms
The Host
Julie Rovner
KFF Health News
Julie Rovner is chief Washington correspondent and host of KFF Health News’ weekly health policy news podcast, “What the Health?” A noted expert on health policy issues, Julie is the author of the critically praised reference book “Health Care Politics and Policy A to Z,” now in its third edition.
The partisan fight in Congress over how to raise the nation’s debt ceiling to prevent a default has accelerated, as the U.S. Treasury predicted the borrowing limit could be reached as soon as June 1. On the table, potentially, are large cuts to federal spending programs, including major health programs.
Meanwhile, legislators in two conservative states, South Carolina and Nebraska, narrowly declined to pass very strict abortion bans, as some Republicans are apparently getting cold feet about the impact on care for pregnant women in their states.
This week’s panelists are Julie Rovner of KFF Health News, Joanne Kenen of the Johns Hopkins Bloomberg School of Public Health and Politico, Rachel Cohrs of Stat, and Alice Miranda Ollstein of Politico.
Panelists
Alice Miranda Ollstein
Politico
Rachel Cohrs
Stat News
Joanne Kenen
Johns Hopkins Bloomberg School of Public Health and Politico
Among the takeaways from this week’s episode:
- The United States is approaching its debt limit — much sooner than expected. And it is unclear how, or if, lawmakers can resolve their differences over the budget before the nation defaults on its debts. Details of the hastily constructed House Republican proposal are coming to light, including apparently inadvertent potential cuts to veterans’ benefits and a lack of exemptions protecting those who are disabled from losing Medicaid and nutrition benefits under proposed work requirements.
- A seemingly routine markup of a key Senate drug pricing package devolved this week as it became clear the committee’s leadership team, under Sen. Bernie Sanders (I-Vt.), had not completed its due diligence to ensure members were informed and on board with the legislation. The Senate Health, Education, Labor and Pensions Committee plans to revisit the package next week, hoping to send it to the full Senate for a vote.
- In more abortion news, Republican lawmakers in North Carolina have agreed on a new, 12-week ban, which would further cut already bare-bones access to the procedure in the South. And federal investigations into two hospitals that refused emergency care to a pregnant woman in distress are raising the prospect of yet another abortion-related showdown over states’ rights before the Supreme Court.
- The number of deaths from covid-19 continues to dwindle. The public health emergency expires next week, and mask mandates are being dropped by health care facilities. There continue to be issues tallying cases and guiding prevention efforts. What’s clear is the coronavirus is not now and may never be gone, but things are getting better from a public health standpoint.
- The surgeon general has issued recommendations to combat the growing public health crisis of loneliness. Structural problems that contribute, like the lack of paid leave and few communal gathering spaces, may be ripe for government intervention. But while health experts frame loneliness as a societal-level problem, the federal government’s advice largely targets individual behaviors.
Plus, for “extra credit,” the panelists suggest health policy stories they read this week they think you should read, too:
Julie Rovner: The Washington Post’s “Dog-Walking Injuries May Be More Common Than You Think,” by Lindsey Bever.
Joanne Kenen: The Atlantic’s “There Is No Stopping the Allergy Apocalypse,” by Yasmin Tayag.
Rachel Cohrs: ProPublica’s “This Pharmacist Said Prisoners Wouldn’t Feel Pain During Lethal Injection. Then Some Shook and Gasped for Air,” by Lauren Gill and Daniel Moritz-Rabson.
Alice Miranda Ollstein: The Wall Street Journal’s “Patients Lose Access to Free Medicines Amid Spat Between Drugmakers, Health Plans,” by Peter Loftus and Joseph Walker.
Also mentioned in this week’s episode:
- The New York Times’ “Surgeon General: We Have Become a Lonely Nation. It’s Time to Fix That,” by Vivek H. Murthy.
- “What the Health?” podcast, July 7, 2022: “A Chat With the Surgeon General on Health Worker Burnout.”
- KFF Health News’ “After Idaho’s Strict Abortion Ban, OB-GYNs Stage a Quick Exodus,” by Sarah Varney.
- Politico’s “‘You Can’t Hide Things’: Feinstein, Old Age and Removing Senators,” by Joanne Kenen.
Click to open the transcript
Transcript: Health Programs Are at Risk as Debt Ceiling Cave-In Looms
KFF Health News’ ‘What the Health?’
Episode Title: Health Programs Are at Risk as Debt Ceiling Cave-In Looms
Episode Number: 296
Published: May 4, 2023
[Editor’s note: This transcript, generated using transcription software, has been edited for style and clarity.]
Julie Rovner: Hello and welcome back to “What the Health?” I’m Julie Rovner, chief Washington correspondent at KFF Health News. And I’m joined by some of the best and smartest health reporters in Washington. We’re taping this week on Thursday, May 4, at 10 a.m. As always, news happens fast and things might have changed by the time you hear this. So here we go. We are joined today via video conference by Joanne Kenen of the Johns Hopkins Bloomberg School of Public Health and Politico.
Joanne Kenen: Hey, everybody.
Rovner: Rachel Cohrs of Stat News.
Rachel Cohrs: Good morning.
Rovner: And Alice Miranda Ollstein of Politico.
Ollstein: Hello.
Rovner: So plenty of news this week. We’re going to dive right in. We’re going to start again this week with the nation’s debt limit, which Treasury Secretary Janet Yellen warned this week could be reached as soon as June 1. That’s a lot earlier than I think most people had been banking on. And if Congress doesn’t act to raise it by then, the U.S. could default on its debts for the first time in history. Do we have any feel yet for how this gets untangled now that we know — I think there are, what, eight days left where both the House and the Senate will be in session?
Ollstein: You said it caught all of us by surprise. It seems to have caught lawmakers by surprise as well. They seem to have thought they had a lot more time to fight and blow smoke at one another, and they really don’t. And there has not been a clear path forward. There are efforts to get Mitch McConnell more involved. He has sort of said, “Ah, you people figure this out. You know, whatever House Republicans and the White House can agree on, the Senate will pass.” And he’s been trying to stay out of it. But now both Republicans and Democrats want him to weigh in. He’s seen as maybe a little more reasonable than some of the House Republicans to some of the players, and so —
Rovner: He may be one of the few Republicans who understands that it would be very, very bad to default.
Ollstein: Right. You have a lot of House Republicans saying it wouldn’t be so bad — the tough medicine for Washington spending, etc. So, you know, if I were to bet money, which I wouldn’t, I would bet on some sort of short-term punt; I mean, we’re really coming up to the deadline, and that’s what Congress loves to do.
Rovner: Yeah, I do too.
Kenen: I agree with Alice. You know, I think if the deadline had been a couple of months from now — they really didn’t want to do a punt. I mean, I think they wanted to walk up to the cliff and cut some kind of deal at the last hour. But I think this caught everybody off guard, including possibly Janet Yellen. So I think it’s much more likely there’ll be a short-term postponement. I think the Democrats would like to tie it to the regular budget talks for the end of the fiscal year. I’m not sure the Republicans will consider September 30 short-term. It might be shorter than that. Of course, we could have another one. But I think Alice’s instincts are right here.
Rovner: Yeah, I do too. I mean, the best thing Congress does is kick the can down the road. They do it every year with all kinds of things. Sorry, Rachel, I interrupted you.
Cohrs: Oh, no, that’s all right. I was just going to flag that the date to watch next week is May 9, when I think they’re all supposed to kind of get in a room together and start this conversation. So I think we’ll hopefully have a readout. I don’t know that they’re going to solve everything in that meeting, but we’ll at least get a sense of where everyone’s coming from and just how acrimonious things really are. So, yeah, those will kick off in earnest.
Rovner: Yeah. Well, one thing the Democrats are talking about is a discharge petition in the House, which is a rarely successful but not all that little-used way to bring a bill to the floor over the objections of the party in charge. Is there any chance that this is going to work this time?
Kenen: That’s one reason the Republicans might not want an extension, because they probably couldn’t do it in the next two or three weeks. There’s a slight chance they could do it in early to mid-June. The Democrats need five Republicans to sign on to that. I would think that if any Republicans are willing to sign on to that, they’re not going to say it in public, so we won’t know who they are, but the chances of it working improve if there’s an extension; the chances of it working are still not great, but I don’t think it’s impossible. I do not think it’s impossible, because there are Republicans who understand that defaulting is not a good idea.
Rovner: This has been painted this week as, Oh, this is a secret idea. It’s like, it’s not, but the actual discharge petition, you get to sign it not anonymously, but no one knows who’s signing on. It’s not like co-sponsoring a regular bill.
Kenen: But stuff gets out. I mean, there’s no such thing as a secret on the Hill.
Rovner: But technically, when you sign it, it’s not an obvious public thing that you’re supporting it, so we will — we’ll have to see. Well, we know that Republicans are demanding deep, in some cases very deep, cuts to federal spending with their bill to raise the debt ceiling. We’re finding out just how deep some of the cuts would be. One possible piece of fallout I think Republicans didn’t bargain for: They say they intended to exempt veterans from the cuts, but apparently the bill doesn’t actually do that, which has already prompted cries of outrage from very powerful veterans groups. This is the danger of these really broadly written bills, right, is that you can sort of actually accidentally end up sweeping in things you didn’t mean to.
Cohrs: Right. Well, this bill came together very quickly, and Kevin McCarthy was dealing with a lot of competing factions and trying to make everyone happy on issues like energy credits, that kind of thing. And obviously this didn’t get attention before. And I think that that’s just kind of a symptom that isn’t infrequent in Washington, where things come together really quickly, and sometimes there are some unintended consequences, but I think that’s one of the functions of kind of the news cycle in Washington especially, is to bring attention to some of these things before they become law. So the rhetoric has been very fiery, but again, there’s a possibility that it could be worked out at a later date if for some reason the final deal ends up looking something like the Republican bill, which is not necessarily the case.
Rovner: Once upon a time — and we’ll talk about this next — we had something called regular order, where bills went through the committee process, there was a committee report, and people had time to look at them before they came to the floor. And now it’s sort of like a fish. If you leave it out too long, it’s going to start to smell. So you got to catch it and pass it right away. Well, before we get to that, another change that those people who wrote the Republican bill probably didn’t intend: The requirement for states to institute work requirements for those who get Medicaid and/or food stamps — something that states cannot opt out of, we are told — does not include exemptions for people with disabilities. In other words, they would be required to work if they are of the age. Even those who’ve been getting, you know, disability benefits for years would have to be recertified as quote “unfit to work” by a doctor, or else they would have their benefits terminated. I would imagine that states would be among those joining the uproar with this. They have enough to do with redeterminations right now from people who got on Medicaid during the pandemic. The last thing they need is to have to basically redetermine every single person who’s already been determined to have a disability.
Kenen: And it’s a burden for the disabled too, even if the states are willing to do it. Bureaucracies are hard to deal with, and people would get lost in the shuffle. There’s absolutely no question that disabled people would get lost in the shuffle given the system they’ve set up.
Ollstein: Yes, this is a perfect example of how people fall through the cracks, and especially because a lot of the mechanisms that states set up to do this, we’ve seen, are not fully accessible for people with disabilities. Some of them have audio-only options. Some of them have online-only options. It’s very hard for people to — even if they know about it, which they might not — to navigate this and become certified. And so there is a fair amount of data out there that the projected savings from policies like work requirements don’t come from more people working; they come from people getting kicked off the rolls who maybe shouldn’t be, should be fully eligible for benefits.
Kenen: And it’s not just physical disability. I mean, there’s all sorts of developmental disabilities — people who really aren’t going to be able to navigate the system. It’s just — it may not be what they intended, it may be what they intended, who knows. But it’s not a viable approach.
Rovner: Yeah. Meanwhile, even if the Democrats could sneak a bill out of the House with a little bit of moderate Republican support, there’s no guarantee it could get through the Senate, where West Virginia’s Joe Manchin says he supports at least some budget cuts and work requirements and where the absence of California’s Dianne Feinstein, who is 89 and has been away from Washington since February, trying to recover from a case of shingles, has loomed large in a body where the elected majority only has 51 votes. Joanne, you wrote about the sticky problem of senators of an advanced age. Feinstein is far from the first, but is there anything that can be done about this when, you know, one of our older senators is out for a long time?
Kenen: There is no institutional solution to an incapacitated senator. And in addition to the magazine piece I wrote about this yesterday for Politico Magazine, I also wrote about last night in Politico Nightly sort of going back to the history until the 1940s. I mean, there have been people, a handful, but people out for like three or four years. The only tool is an expulsion vote, and that is not used. You need two-thirds vote, and you can’t get that. It was used during the Civil War, where there were I think it was 14 senators from Confederate states who didn’t sort of get that they were supposed to leave once the Civil War started, so they got expelled. Other than that, there’s only been one case, and it was for treason, in the 1790s. So they’re not going to start expelling senators who have strokes or who have dementia or who have other ailments. That’s just not going to happen. But that means they’re stuck with them. And it’s not just Feinstein. I mean, there have been other impaired senators, and there will be more impaired senators in the future. There’s no equivalent to the 25th Amendment, for which the vice president and the cabinet can remove a president. The Senate has no mechanism other than behind-the-scenes cajoling. And, you know, we have seen Dianne Feinstein — she didn’t even announce she wasn’t running for reelection until other people announced they were running for her seat. But it’s like 50-50 Senate — if it’s 47-53 and one is sick, it doesn’t matter so much. If it’s 50-50 or 51-49, it matters a lot.
Rovner: Yeah, and that’s what I was going to say. I mean, you and I remember when Tim Johnson from South Dakota had, what was it, an aneurysm?
Kenen: I think he had a stroke, right?
Rovner: Yeah. It took him a year to come back, which he did eventually.
Kenen: Well, we both covered Strom Thurmond, who, you know, was clearly not —
Rovner: —he was not all there —
Kenen: — situational awareness for quite a few years. I mean, it was very clear, you know, as I mention in this story, that, you know, instead of the staff following his orders, he was following the staff’s orders and he was not cognizant of Senate proceedings or what was going on.
Rovner: Yeah, that’s for sure.
Kenen: But there also are some who are really fine. I mean, we know some who are 80, 88 — you know, in their 80s who are totally alert. And so an age cutoff is also problematic. That doesn’t work either.
Rovner: Right. Ted Kennedy was, you know, right there until he wasn’t. So I’m amazed at the at how some of these 80-something-year-old senators have more energy than I do. Well, elsewhere on Capitol Hill, we talked about the bipartisan drug price bill last week in the Senate that was supposed to be marked up and sent to the floor this week, which did not happen. Rachel, how did what should have been a fairly routine committee vote get so messed up?
Cohrs: Yeah, it was a — it was a meltdown. We haven’t seen something like this in quite a — a couple of years, I think, on the Hill, where Chairman Bernie Sanders’ first major, you know, health care markup. And I think it just became clear that they had not done due diligence down the dais and had buy-in on these bills, but also the amendment process, which sounds like a procedural complaint but it really — there were some substantive changes in these amendments, and it was obvious from the markup that senators were confused about who supported what and what could get the support of the caucus. And those conversations in the Lamar Alexander, you know, iteration of this committee happened before. So I think it, you know, was a lesson certainly for everyone that there does need to be — I don’t know, it’s hard to draw the line between kind of regular order, where every senator can offer an amendment, and what passes. And it’s just another symptom of that issue in Congress where even sometimes popular things that an individual senator might support — they could pass on their own — that throwing off the dynamics of packages that they’re trying to put together. So I think they are hoping to give it another shot next week after a hearing with executives from insulin manufacturers and pharmacy benefit managers. But it was pretty embarrassing this week.
Rovner: Yeah. I was going to say, I mean normally these things are negotiated out behind the scenes so by the time you actually — if you’re going to have a markup; sometimes markups get canceled at the last minute because they haven’t been able to work things out behind the scenes. Correct me if I’m wrong, but Bernie Sanders has not been chairman before of a major legislative committee, right? He was chairman of the Budget Committee, but they don’t do this kind of take up a bill and make amendments.
Kenen: I don’t remember, but he was a lead author of the bipartisan veterans bill. So he has — it’s probably his biggest legislative achievement in the Senate. And that was a major bipartisan bill. So he does know how these things work.
Rovner: Right. He knows how to negotiate.
Kenen: It just didn’t work.
Rovner: Yeah, I think this came as a surprise — a committee like this that’s really busy with legislation and that does legislation that frequently gets amended and changed before it goes to the floor. I am told he was indeed chairman of Veterans’ Affairs, but they don’t do as much legislation as the HELP Committee. I think this was perhaps his first outing. Maybe he learned some important lessons about how this committee actually works and how it should go on. All right. Rachel, you said that there’s going to be a hearing and then they’re going to try this markup again. So we’ll see if they get through this in the May work period, as they call it.
Kenen: Maybe they’ll come out holding hands.
Rovner: I want to turn to abortion. It seems that maybe, possibly, the tide in states is turning against passage of the broadest possible bans. In the same day last week we saw sweeping abortion restrictions turned back, though barely, by lawmakers in both South Carolina and Nebraska. And in North Carolina, where Republicans just got a supermajority big enough to override the state’s Democratic governor’s veto, lawmakers are now looking at a 12-week ban rather than the six-week or total ban that was expected. Alice, is this a trend or kind of an anomaly?
Ollstein: Every state is different, and you still have folks pushing for total or near-total bans in a lot of states. And I will say that in North Carolina specifically, a 12-week ban will have a big impact, because that is the state where a lot of people throughout the entire South are going right now, so they’re getting incoming folks from Texas, Oklahoma, Alabama, Louisiana. So it’s one of the sort of last havens in the entire southeast area, and so even a restriction to 12 weeks, you know, we know that the vast majority of abortions happen before that point, but with fewer and fewer places for people to go, wait times are longer, people are pushed later into pregnancy who want to terminate a pregnancy sooner. And so it could be a big deal. This has also been kind of a crazy saga in North Carolina, with a single lawmaker switching parties and that being what is likely to enable this to pass.
Rovner: Yeah, a Democrat turned Republican for reasons that I think have not been made totally clear yet, but giving the Republicans this veto-proof majority.
Kenen: They’ve got the veto-proof majority. I did read one report saying there was one vote in question. It might be this lawmaker who turned, whether she’s for 12-week or whether she’s for 15 or 20 or whatever else. So it’ll certainly pass. I don’t have firsthand knowledge of this, but I did read one story that said there’s some question about they might be one short of the veto-proof majority. So we’ll just have to wait and see.
Rovner: Yeah, North Carolina is obviously a state that’s continuing. So my colleague and sometime podcast panelist Sarah Varney has a story this week out of Idaho, where doctors who treat pregnant women are leaving the state and hospitals are closing maternity wards because they can no longer staff them. It’s a very good story, but what grabbed me most was a line from an Idaho state representative who voted for the ban, Republican Mark Sauter. He told Sarah, quote, “he hadn’t thought very much about the state abortion ban other than I’m a pro-life guy and I ran that way.” He said it wasn’t until he had dinner with the wife of a hospital emergency room doctor that he realized what the ban was doing to doctors and hospitals in the state and to pregnant women who were not trying to have abortions. Are we starting to see more of that, Alice? I’ve seen, you know, a few Republicans here and there saying that — now that they’re seeing what’s playing out — they’re not so sure these really dramatic bans are the way to go.
Ollstein: Yeah, I will say we are seeing more and more of that. I’ve done some reporting on Tennessee, where some of the Republicans who voted for the state’s near-total ban are expressing regret and saying that there have been unintended consequences for people in obstetric emergency situations. You know, they said they didn’t realize how this would be a chilling effect on doctors providing care in more than just so-called elective abortion situations. But it does seem that those Republicans who are speaking out in that way are still in the majority. The party overall is still pushing for these restrictions. They’re also accusing medical groups of misinterpreting them. So we are seeing this play out. For instance, you know, in Tennessee, there was a push to include more exceptions in the ban, alter enforcement so that doctors wouldn’t be afraid to perform care in emergency situations, and a lot of that was rejected. What they ended up passing didn’t go as far as what the medical groups say is needed to protect pregnant people.
Rovner: It’s important to point out that the groups on the other side, the anti-abortion groups, have not backed off. They are still — and these are the groups that have supported most of these pro-life Republicans who are in these state legislatures. So were they to, you know, even support more exemptions that would, you know, turn them against important supporters that they have, so I think it’s this —
Ollstein: —right—
Rovner: —sort of balancing act going on.
Ollstein: Plus, we’ve seen even in the states that have exemptions, people are not able to use them in a lot of circumstances. That’s why you have a lot of pro-abortion rights groups, including medical groups, saying exemptions may give the appearance of being more compassionate but are not really navigable in practice.
Rovner: Right. I mean, we’ve had all these stories every week of how near death does a pregnant woman have to be before doctors are not afraid to treat her because they will be dragged into court or put in jail?
Ollstein: Right.
Rovner: So this continues. Well, the other big story of the week has to do with exactly that. The federal Department of Health and Human Services has opened an investigation into two hospitals, one each in Missouri and Kansas, that federal officials say violated the federal emergency medical care law by refusing to perform an abortion on a woman in medical distress. If the hospitals don’t prove that they will comply with the law, they could face fines or worse, be banned from participation in Medicare and Medicaid. I can’t help but think this is the kind of fight that’s going to end up at the Supreme Court, right? I mean, this whole, if you have a state law that conflicts with federal law, what do you do?
Ollstein: Yeah, we’re seeing that both in the EMTALA space [Emergency Medical Treatment and Labor Act] and in the drug space. We’re seeing a lot of state-federal conflicts being tested in court, sort of for the first time in the abortion question. So we also, in addition to these new federal actions, you know, we still have cases playing out related to abortion and emergency care in a few other states. So I think this will continue, and I think that you’re really seeing that exactly the letter of the law is one thing, and the chilling effect is another thing. And how doctors point out if a lot of these state abortion bans are structured around what’s called an affirmative defense, which means that doctors have to cross their fingers and provide the care and know that if they get sued, they can mount a defense that, you know, this was necessary to save someone’s life. Now, doctors point out that a lot of people are not willing to do that and a lot of people are afraid to do that; they don’t have the resources to do it. Plus, in the medical space, when you apply for licenses or things in the future, it doesn’t just say, “Were you ever convicted of something?” It says, “Were you ever charged with something?” So even if the charges are dropped, it still remains on their record forever.
Rovner: Yeah, and they have malpractice premiums. I mean, there’s a whole lot of things that this will impact. Well, I want to talk about covid, because we haven’t talked about covid in a couple of weeks. It is still with us. Ask people who went to the big CDC conference last week; I think they’ve had, what, 35 cases out of that conference? Yet the public health emergency officially ends on May 11, which will trigger all manner of changes. We’re already seeing states disenrolling people for Medicaid now that they’re allowed to redetermine eligibility again, including some people who say they’re still eligible, as we talked about a little bit earlier. We’re also seeing vaccine mandates lifted. Does this mean that the pandemic is really over? It obviously is a major signal, right, even if covid is still around?
Kenen: It means it’s legally over. It doesn’t mean it’s biologically over. But it is clearly better. I mean, will we have more surges next winter or over some kind of holiday gathering? You know, it’s not gone and it’s probably never going to be gone. However, we also don’t know how many cases there really are because not everybody tests or they don’t realize that cold is covid or they test at home and don’t report it. So the caseload is murky, but we sure note that the death toll is the lowest it’s been in two years, and I think it’s under 200 a day — and I’d have to double check that — but it’s really dropped and it’s continuing to drop. So even though there’s concern about whether we still need some of these protections, and I personally think we do need some of them in some places, the bottom line is, are people dying the way they were dying? No. That is — you know, I’ve watched that death toll drop over the last couple of weeks; it’s consistent and it’s significant. And so we should all be grateful for that. But whether it stays low without some of these measures and access to testing and access to shots and — and people are confused, you know, like, Oh, the shots aren’t going to be free or they are going to be free or I don’t need one. I mean, that whole murkiness on the part of the public — I mean, I have friends who are quite well aware of things. I mean, I have friends who just got covid the other day and, you know, said, “Well, you know, I’m not going to — I’m not really, really sick, so I don’t need Paxlovid.” And I said, “You know, you really need to call your doctor and talk about that.” So her doctor gave her Paxlovid — so she actually had a risk factor, so, two risk factors. So it’s not over, but we also have to acknowledge that it’s better than many people thought it would be by May 2023.
Rovner: Yeah, I know. I mean, the big complaints I’m seeing are people with chronic illnesses who worry that masks are no longer required in health care facilities, and that that seems to upset them.
Kenen: I mean, I think if you were to ask a doctor, I would hope that you could ask your doctor to put on a mask in a certain situation. And that doesn’t work in a hospital where lots of people around, but the doctors I’ve been to recently have also worn masks and —
Rovner: Yeah, mine too.
Kenen: Luckily, we do know now that if you wear a good mask, an N95, properly, it is not perfect, but you still can protect yourself by wearing a mask. You know, I take public transport and I wear masks in public transport, and I still avoid certain settings, and I worry more about the people who are at risk and they don’t understand that the shots are still free; they don’t know how to get medication; they don’t — there’s just a lot of stuff out there that we have communicated so poorly. And the lack of a public health emergency, with both the resources and the messaging — I worry about that.
Rovner: And as we pointed out, people losing their health insurance, whether, you know —
Kenen: That’s a whole other —
Rovner: Yeah, rightly or not. I mean, you know, whether they’re no longer eligible.
Kenen: Most are, but they’re still, you know — falling through the cracks is a major theme in American health care.
Rovner: It is. Well, finally this week, the U.S. surgeon general, Vivek Murthy, wants us to be less lonely. Really. The health effects of loneliness have been a signature issue for Dr. Murthy. We talked about it at some length in a podcast last summer. I will be sure to add the link to that in the show notes. But now, instead of just describing how loneliness is bad for your health — and trust me, loneliness is bad for your health — the surgeon general’s office has issued a new bulletin with how Americans can make themselves less lonely. It’s not exactly rocket science. It recommends spending more time in person with friends and less time online. But does highlighting the issue make it easier to deal with? I mean, this is not one of the traditional public health issues that we’ve talked about over the years.
Ollstein: I’m very interested to see where this conversation goes, because it’s already sort of feeling like a lot of other public health conversations in the U.S. in that they describe this huge, existential, population-level problem, but the solutions pushed are very individual and very like, you have to change your lifestyle, you have to log off, you have to join more community groups. And it’s like, if this is a massive societal problem, shouldn’t there be bigger, broader policy responses?
Kenen: You can’t mandate someone going out for coffee —
Ollstein: —exactly—
Kenen: —three times a week. I mean, this one —
Ollstein: Exactly. You can’t boostrap loneliness.
Kenen: This one, I think — I think it validates people’s feelings. I mean, I think people who are feeling isolated —I mean, we had loneliness before the pandemic, but the pandemic has changed how we live and how we socialize. And if — I think it’s sort of telling people, you know, if you’re feeling this way, it is real and it’s common, and other people are feeling that way, too, so pick up the phone. And maybe those of us who are more extroverted will reach out to people we know who are more isolated. So, I mean, I’m not sure what HHS or the surgeon general can do to make people spend time with one another.
Ollstein: Well, there are structural factors in loneliness. There are economic factors. There is, you know, a lack of paid time off. There are a lack of public spaces where people can gather, you know, in a safe and pleasant way. You know, other countries do tons of things. You know, there are programs in other countries that encourage teens, that finance and support teens forming garage bands, in Scandinavian countries. I mean, there are there are policy responses, and maybe some of them are already being tried out at like the city level in a lot of places. But I’m not hearing a lot other than telling people to make individual life changes, which may not be possible.
Rovner: But although I was going to point out that one of the reasons that this is becoming a bigger issue is that the number of Americans living alone has gone up. You know, and again, Joanne, this was way before the pandemic, but it’s more likely — people are more in a position to be lonely, basically. I mean, it’s going to affect a larger part of the population, so —
Kenen: And some of the things that Alice suggested are policies that are being worked on because of, you know, social determinants and other things: recreation, housing. Those things are happening at both the state and federal level. So they would help loneliness, but I don’t think you’re going to see them branded as a loneliness — national loneliness program. But, you know, the demographics of this country — you know, families are scattered. Zoom is great, you know, but Zoom isn’t real life. And there are more people who are single, there are more people who are widowed, there are more people who never married, there are more people who are divorced, the elderly cohort. Many people live alone, and teens and kids have had a hard time in the last couple years. So I think on one level it’s easy for people to make fun of it because, you know, we’re coming out of this pandemic and the surgeon general’s talking about loneliness. On the other hand, there are millions or tens of millions of people who are lonely. And I think this does sort of help people understand that there are things to be done about it that — I don’t think individual action is always a bad thing. I mean, encouraging people to think about the people in their lives who might be lonely is probably a good thing. It’s social cohesion. I mean, Republicans can make that case, right, that we have to, you know, everybody needs to pick up a telephone or go for a walk and knock on a door.
Rovner: Yeah, they do. I mean, Republicans are big on doing things at the community level. That’s the idea, is let’s have government at the lowest level possible. Well, this will be an interesting issue to watch and see if it catches on more with the public health community. All right. That is this week’s news. Now it is time for our extra credit segment. That’s when we each recommend a story we read this week we think you should read too. As always, don’t worry if you miss it. We will post the links on the podcast page at KFF Health News and in our show notes on your phone or other mobile device. Rachel, why don’t you go first this week?
Cohrs: My story is in ProPublica and the headline is “This Pharmacist Said Prisoners Wouldn’t Feel Pain During Lethal Injection. Then Some Shook and Gasped for Air,” by Lauren Gill and Daniel Moritz-Rabson. And I think it’s just a story about this ongoing issue of expert testimony in criminal justice settings. And obviously these are really important questions about medications that, you know, are used for lethal injections and how they work and just how, you know, people are responding to them in the moment. And I mean, it’s just such an important issue that gets overlooked in the pharmaceutical space sometimes. And yeah, I think it’s just something that is very sobering, and it’s just a really important read.
Rovner: Yeah. I mean, there’s been a lot about doctors and the ethics of participating in these. This is the first time I’ve seen a story about pharmacists. Joanne?
Kenen: Well, I saw this one in The Atlantic. It’s by Yasmin Tayag, and I couldn’t resist the headline: “There Is No Stopping the Allergy Apocalypse.” Basically, because of climate change, allergies are getting worse. If you have allergies, you already know that. If you think you don’t have allergies, you’re probably wrong; you’re probably about to get them. They take a little while to show up. So it’s not in one region; it’s everywhere. So, you know, we’re all going to be wheezing, coughing, sneezing, sniffling a lot more than we’re used to, including if you were not previously a wheezer, cougher, or sniffler.
Rovner: Oh, I can’t wait. Alice.
Ollstein: So I have a piece from The Wall Street Journal called “Patients Lose Access to Free Medicines Amid Spat Between Drugmakers, Health Plans,” by Peter Loftus and Joseph Walker. And it is some really tragic stories about folks who are seeing their monthly costs for medications they depend on to live shoot up. In one instance in the story, what he has to pay per month shot up from 15 to more than 12,000. And so you have the drugmakers, the insurance companies, and the middlemen pointing fingers at each other and saying, you know, “This is your fault, this is your fault, this is your fault.” And meanwhile, patients are suffering. So, really interesting story, hope it leads to some action to help folks.
Rovner: I was going to say, maybe the HELP Committee will get its act together, because it’s trying to work on this.
Ollstein: Yeah.
Rovner: Well, my story is from The Washington Post, and it’s called “Dog-Walking Injuries May Be More Common Than You Think,” by Lindsey Bever. And it’s about a study from Johns Hopkins, including your colleagues, Joanne, that found that nearly half a million people were treated in U.S. emergency rooms for an injury sustained while walking a dog on a leash. Not surprisingly, most were women and older adults, who are most likely to be pulled down by a very strong dog. The three most diagnosed injuries were finger fractures, traumatic brain injuries, and shoulder injuries. As a part-time dog trainer in my other life, here are my two biggest tips, other than training your dog to walk politely on a leash: Don’t use retractable leashes; they can actually cut off a finger if it gets caught in one. And never wrap the leash around your hand or your wrist. So that is my medical advice for this week. And that is our show. As always, if you enjoy the podcast, you can subscribe wherever you get your podcasts. We’d appreciate it if you left us a review; that helps other people find us too. Special thanks, as always, to our ever-patient producer, Francis Ying. Also, as always, you can email us your comments or questions. We’re at whatthehealth@kff.org. Or you can tweet me, as long as Twitter’s still there. I’m @jrovner. Joanne?
Kenen: @JoanneKenen.
Rovner: Alice.
Ollstein: @AliceOllstein.
Rovner: Rachel.
Cohrs: @rachelcohrs.
Rovner: We will be back in your feed next week. Until then, be healthy.
Credits
Francis Ying
Audio producer
Emmarie Huetteman
Editor
To hear all our podcasts, click here.
And subscribe to KFF Health News’ ‘What the Health? on Spotify, Apple Podcasts, Stitcher, Pocket Casts, or wherever you listen to podcasts.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
2 years 3 months ago
Capitol Desk, Courts, COVID-19, Health Care Reform, Health Industry, Insurance, Medicaid, Medicare, Mental Health, Multimedia, Public Health, Abortion, Biden Administration, KFF Health News' 'What The Health?', North Carolina, Podcasts, Women's Health
El dolor, la esperanza y la ciencia chocan cuando los atletas recurren a los hongos mágicos
WAKEFIELD, Jamaica — El boxeador se sentía destrozado. Todos los días, se despertaba con dolor. A veces eran dolores de cabeza debilitantes. Otros, era su espalda. O sus puños. Sus costillas. Su nariz. Además, sufría de cambios de humor. Depresión. Ansiedad.
Mike Lee no se arrepintió de su carrera. Había sido uno de los mejores boxeadores profesionales del mundo en su categoría. Tenía marca de 21-1, y peleó en el Madison Square Garden y frente a millones en la televisión.
Pero habían pasado más de dos años desde que pisó un ring, y cada día era un recordatorio del costo. En un momento, Lee estaba tomando ocho medicamentos recetados, todos para tratar de sobrellevar la situación.
Contó que, en su momento más bajo, en una noche en que estaba en lo más profundo de una adicción a los analgésicos, pensó en chocar su auto contra la valla de una autopista de Chicago a 140 mph.
Estaba dispuesto a hacer cualquier cosa para escapar del infierno en el que se sentía atrapado.
El impulso se desvaneció, pero el dolor permaneció.
Estaba perdido.
“Cuando tienes dolor y estás atrapado, harás cualquier cosa para salir de eso”, dijo Lee.
Ahora, había llegado a una jungla verde al final de un camino de tierra en la mitad de una montaña.
Esperaba que los hongos psicodélicos pudieran cambiar su vida.
Lee era parte de un pequeño grupo, muchos de ellos atletas retirados, que viajaron a Jamaica en marzo de 2022 para un retiro que costó hasta $5500. Cada uno de ellos había venido a Good Hope Estate, una plantación de azúcar convertida en centro turístico exclusivo, con la esperanza de librarse de la depresión, la ansiedad y el dolor crónico que habían experimentado durante años.
Dos ceremonias con hongos psicodélicos y dos sesiones de terapia les esperaban en el retiro dirigido por una empresa canadiense llamada Wake Network. Los participantes estaban nerviosos, pero también esperanzados.
Junto con Lee, había un jugador profesional de fútbol americano que estaba considerando retirarse y una ex estrella de hockey que tenía múltiples conmociones cerebrales.
Venían de todas partes de América del Norte, de diferentes orígenes y diferentes deportes, pero tenían algunas cosas en común: eran vulnerables y sentían que los medicamentos recetados les habían fallado. No sabían qué esperar, si el tratamiento funcionaría, si regresarían a casa con una solución o simplemente con otra decepción.
Lee se enteró del retiro por un amigo de la infancia que trabaja como médico en Wake. Otros habían sido reclutados por Riley Cote, un ex ejecutor de los Philadelphia Flyers y ahora un evangelista psicodélico que es asesor de Wake con una participación accionaria.
Alguna vez, Cote fue como Lee. Le encantaba golpear a la gente en la cara. Amaba la forma en que su mano aterrizaba con un ruido sordo cuando sus nudillos se conectaban con la carne y el hueso a una velocidad violenta. Romper la cabeza de alguien hacía que Cote se sintiera vivo.
“Luché contra todos. Escogía al tipo más grande que pudiera encontrar y lo desafiaba. Así fue como sobreviví, cómo me hice un nombre. Me estaba infligiendo todo este dolor e inflamación, siempre recibiendo puñetazos en la cara, y tenía que mantener este tipo de personalidad machista, como, ‘Oh, no puedes lastimarme. No puedes lastimarme’”.
Ya no era esa persona. Le daba escalofríos pensar en el hombre que alguna vez fue, alguien que bebía en exceso y usaba analgésicos para adormecer su cerebro. Hubo un tiempo en que él, como Lee, estaba en un lugar oscuro, pero con el transcurso de varios años, los hongos psicodélicos, cree Cote, lo ayudaron a regresar a la luz.
“El mundo está en una crisis, una crisis de salud mental, una crisis espiritual”, dijo Cote. “Y creo que estas son medicinas espirituales, y siento que es el camino correcto para mí. No lo considero más que mi deber, mi propósito en este planeta es compartir la verdad sobre la medicina natural”.
Durante años, han circulado rumores sobre una red clandestina de atletas, principalmente ex atletas, que usan psilocibina, el compuesto de los hongos mágicos, para tratar lesiones cerebrales traumáticas, ansiedad y depresión.
Muchos de ellos, como Cote, ven a los psicodélicos como una cura milagrosa, lo único que pudieron encontrar que podría ayudar a romper un ciclo de analgésicos y abuso de sustancias. Se reunían en pequeños grupos para ingerir hongos en privado o viajaban a países como Jamaica donde los hongos psicodélicos no están prohibidos.
Ahora, el uso de hongos psicodélicos está ganando terreno en los Estados Unidos. Varias ciudades han despenalizado la posesión de psilocibina, y los votantes de Oregon y Colorado aprobaron medidas electorales para legalizar los hongos mágicos bajo uso supervisado. Muchos investigadores predicen que la Administración de Drogas y Alimentos (FDA) aprobará un tratamiento psicodélico en los próximos cinco años.
Pero muchos de esos mismos investigadores advierten que la intensa promoción de los psicodélicos está superando a la ciencia, y que el tratamiento conlleva riesgos significativos para algunos pacientes. Temen que, a menos que la investigación se lleve a cabo de forma metódica y ética, el uso generalizado de la psilocibina podría resultar en una reacción negativa del público, como sucedió en la década de 1960, relegando un tratamiento prometedor al basurero de las sustancias prohibidas.
Están instando a las entidades corporativas como Wake, que ya se están posicionando para aprovechar la posible legalización de los psicodélicos, a que avancen lentamente, se aseguren de que la investigación se realice de la manera correcta y permitan que la ciencia se ponga al día.
“Si no haces esto de manera segura, la gente saldrá lastimada”, dijo Matthew Johnson, profesor de psiquiatría e investigador de psicodélicos en la Universidad Johns Hopkins.
Pero muchos, incluidos los ex atletas profesionales con cuerpos y cerebros maltratados, no quieren esperar el lento avance de la investigación clínica. Necesitan ayuda ahora.
Los analgésicos, los antidepresivos, las innumerables píldoras diferentes que les recetaron a lo largo de los años no han ayudado. En sus mentes, las historias de sus compañeros atletas que dicen que se han beneficiado de los psicodélicos superan cualquier incertidumbre científica.
“Cuando piensas en hongos mágicos, piensas en los hippies de Woodstock bailando al ritmo de la música”, dijo Lee. “Pensar que tienes algunos de los mejores atletas del mundo aquí que están lidiando con algunas cosas y las están tomando, te hace sentir más cómodo. Me hace sentir como, ‘Está bien, tal vez estoy haciendo lo correcto’. Es una medicina curativa; no es solo una droga de fiesta”.
***
Cote, ahora de 41 años, era un patinador de hockey decente que creció en Winnipeg, Manitoba, tenaz de punta a punta y un trabajador incansable, pero bastante promedio en el manejo del disco.
No anotó suficientes goles para ascender en el hockey junior como lo hicieron algunos prospectos. Sin embargo, a medida que crecía, a los entrenadores no les importaba tanto. Tenía hombros anchos y un largo alcance. En una era del hockey en la cual la violencia todavía era moneda corriente, había encontrado su boleto dorado para la NHL: Cote golpeaba a la gente y recibía golpes a cambio.
Como miembro de los Flyers, vio que era su deber mantener las tradiciones de los Broad Street Bullies, un grupo de jugadores de la década de 1970 que fueron celebrados por la prensa por jugar y festejar fuerte.
Se abrió camino a través de la NHL durante partes de cuatro temporadas, acumulando más de 400 minutos de penalización en su carrera y anotando solo un gol. La mayoría de sus peleas fueron situaciones brutales, bárbaras. Sus destacados muestran a un gigante corpulento, con los ojos llenos de violencia, el tipo de matón que podría romperte la mandíbula y reír como un maníaco después, la sangre goteando de su rostro y cayendo al hielo.
“Fue algo que disfruté hacer, y creo que era solo un elemento de competencia para mí”, dijo Cote. “Y probablemente también era algo que estaba haciendo por miedo: miedo de no vivir mi sueño de la infancia o de decepcionar a mis padres o a la gente”.
Dijo que se medicaba por su dolor casi todos los días con alcohol. Las cervezas eran un aperitivo de camino a los shots en la barra. Después, venían drogas duras. Él y sus compañeros de equipo se quedaban fuera hasta las 3 am, a veces más tarde, y luego intentaban sudar el veneno al día siguiente durante la práctica.
Después de unos años, su cerebro comenzó a empañarse. Se hizo más grande y más fuerte a través del levantamiento de pesas, y parecía un monstruo en el hielo, pero cada una de sus habilidades de hockey se deterioró, salvo las peleas. A medida que su carrera terminaba, dijo, se sentía como si la oscuridad se acercara sigilosamente. Se deprimió. Tenía miedo de en lo que se había convertido.
Hoy, Cote se parece poco a aquel ejecutor de los videos. Más delgado y tranquilo, imparte clases de yoga en un estudio de Delaware tres veces por semana. Con el pelo hasta los hombros, tatuajes en los brazos y el pecho, habla con una suave voz de barítono. Parece más un monje que un monstruo.
“Miro hacia atrás y tal vez solo muestra lo confundido que estaba y la realidad que estaba buscando, que supuestamente era la felicidad y la satisfacción de perseguir el sueño de mi infancia”, dijo Cote. “Pero es difícil para mí entender que estoy haciendo eso ahora, simplemente sabiendo quién soy ahora y dándome cuenta de que se necesita mucha oscuridad para hacer lo que hice”.
Cote dijo que tomó hongos de forma recreativa durante sus 20 años, pero nunca en un entorno terapéutico o con el entendimiento de que podrían ayudarlo a procesar su trauma físico y emocional. “Era solo parte de la escena o parte de la fiesta”, dijo.
Pero cuando se jubiló en 2010, sintió que estaba enfrentando una crisis de identidad. Había sido un luchador durante tanto tiempo que pensó que eso era todo lo que era. ¿Cómo podría un ejecutor fracasado criar a dos hijas?
Empezó a leer. Lo que aprendió lo sorprendió.
Los investigadores habían revivido silenciosamente el estudio sobre los hongos psicodélicos como tratamiento médico en el año 2000, y los primeros hallazgos sugirieron que la psilocibina a menudo tenía beneficios notables para las personas diagnosticadas con ansiedad y depresión. Ayudó a algunos pacientes a deshacerse de sus adicciones a las drogas o al alcohol.
Otra investigación sugirió que la psilocibina en realidad puede ser capaz de remodelar la anatomía del cerebro, restaurar las vías neurológicas y ayudar a curar lesiones cerebrales traumáticas.
Para Cote, a quien le diagnosticaron al menos tres conmociones cerebrales en su carrera de hockey y probablemente sufrió muchas más, fue transformador.
Cote ahora recluta clientes para Wake, que organiza retiros inmersivos de psilocibina fuera de los Estados Unidos.
“Algunas personas vienen a estos eventos y están al borde del suicidio”, dijo Tyler Macleod, cofundador de Wake y su director de experiencia. “No se arreglan después de una ceremonia, pero ya no están atascados en la oscuridad. Se despiertan y dicen: ‘Oh, puedo navegar de nuevo una relación con mis hijos'”.
Todos los ex atletas que asisten a estos retiros están luchando con algo, dijo Cote. Necesitan ayuda. En muchos casos, sienten que han probado todo lo demás. Les pregunta por qué tienen que esperar cuando tantos estudios y anécdotas indican resultados positivos.
“Es como con el cannabis: ¿cuántas historias tuvimos que contarnos antes de tener un programa médico?”, apuntó Cote. “Simplemente ha estado bloqueado durante tanto tiempo”.
***
En 1970, el presidente Richard Nixon promulgó la Ley de Sustancias Controladas, legislación que dividía las drogas en cinco niveles, clasificándolas en gran medida según su potencial de abuso. Los hongos mágicos se clasificaron como sustancias de la Lista 1, junto con la heroína y la marihuana, lo que significa que el gobierno creía que no tenían ningún beneficio médico y que tenían un alto potencial de generar adicción. (La cocaína, la oxicodona y la metanfetamina se clasificaron como drogas de la Lista 2).
Esas decisiones, que el asesor de Nixon, John Ehrlichman, dijo más tarde que tenían motivaciones políticas, continúan teniendo un efecto dominó en la actualidad. La investigación sobre tratamientos psicodélicos se suspendió durante 30 años.
Si bien los estudios recientes han tenido un alcance pequeño, han mostrado efectos notables. Los medicamentos recetados aprobados para afecciones como la ansiedad o la depresión ayudan, en el mejor de los casos, a entre el 40% y el 60% de los pacientes. En los primeros ensayos, los psicodélicos han alcanzado tasas de eficacia de más del 70%.
Y, a diferencia de la mayoría de los medicamentos recetados, que dejan de funcionar poco después de que los pacientes dejan de tomarlos, uno o dos tratamientos de psilocibina pueden tener efectos terapéuticos por seis meses, un año o incluso más, según un estudio de Johns Hopkins.
Con un riesgo mínimo de adicción o sobredosis y siglos de uso por parte de las culturas indígenas, muchos investigadores consideran que la psilocibina es un tratamiento innovador potencial con grandes beneficios y pocos riesgos.
Scott Aaronson, director de programas de investigación clínica en Sheppard Pratt, un hospital psiquiátrico sin fines de lucro en las afueras de Baltimore, ha estado estudiando los trastornos del estado de ánimo difíciles de tratar durante 40 años, comenzando con algunos de los primeros estudios sobre Prozac.
“Soy un ser humano cínico, escéptico y sarcástico”, dijo Aaronson. “Y te diré, nunca he visto algo así en todos mis años”.
Pero la psilocibina no está exenta de riesgos. Puede exacerbar problemas cardíacos y desencadenar esquizofrenia en personas con una predisposición genética, y la combinación de psilocibina y litio puede causar convulsiones.
Los ensayos clínicos generalmente han descartado a los pacientes en riesgo de tales complicaciones. Aún así, una parte significativa de quienes consumen psilocibina, incluso sin ninguna de esas preocupaciones, tienen una experiencia negativa.
“En una dosis alta, alrededor de un tercio de las personas en nuestros estudios, incluso en estas condiciones ideales, pueden tener lo que se llamaría un mal viaje, algún grado de ansiedad o miedo sustancial”, dijo Johnson, investigador de Johns Hopkins. “Una persona puede ser muy vulnerable psicológicamente. Puede sentirse como si estuvieran muriendo”.
Sin embargo, a veces, incluso esos “malos viajes” pueden conducir a la ayuda con la depresión u otros problemas, según han descubierto investigadores, especialmente con la ayuda de seguimiento de un terapeuta para procesar la experiencia.
Los efectos psicodélicos de la psilocibina también pueden desconectar a una persona de la realidad, lo que puede llevar a las personas a hacer cosas peligrosas, como correr hacia el tráfico o saltar por una ventana.
“La percepción misma de la realidad y de ellos mismos en la realidad, como quiénes son, estas cosas pueden cambiar profundamente y no es una buena receta para interactuar en público”, dijo Johnson.
Los investigadores también describen casos en los que la psilocibina pone a las personas con problemas psicológicos no resueltos en estado de angustia a largo plazo.
Es por eso que los investigadores insisten en que la psilocibina debe administrarse en un entorno clínico con terapeutas capacitados que puedan guiar a las personas a través de la experiencia, lidiar con los resultados negativos cuando surjan, y ayudarlas a procesar e integrar sus experiencias.
Los ensayos clínicos de psilocibina se han basado en protocolos estrictos, que incluyen una o más sesiones antes del tratamiento para ayudar a los participantes a comprender qué esperar. El consumo de los hongos se hace a menudo en un solo día, con uno o dos terapeutas disponibles.
En los días siguientes, la persona regresa para lo que se conoce como integración, generalmente una sesión de terapia individual para ayudar a procesar la experiencia y comenzar el camino hacia la curación. Algunos ensayos agregan un día adicional de terapia entre dos tratamientos.
A diferencia de un medicamento típico, nose envía a los pacientes a casa con un frasco de píldoras. Todo el protocolo se parece más a un procedimiento médico.
Pero es un error pensar que es la medicina psicodélica la que hace todo el trabajo, no la terapia que viene después, dijo Jeffrey LaPratt, psicólogo e investigador de psilocibina con Sheppard Pratt. “Es un trabajo muy duro y requiere vulnerabilidad. Se necesita coraje. Puede ser realmente doloroso”.
***
El ex jugador de la NHL Steve Downie sintió como si algo en él se hubiera roto cuando lo invitaron al retiro de Wake en Jamaica. Sus días estaban llenos de niebla. Vivía con depresión, a menudo incapaz de salir de su casa.
“Me cansé de ir a esos médicos y me cansé de hablar con ellos”, dijo Downie. “No me malinterpreten, no digo que los médicos sean malos. Solo digo que, en mi experiencia personal, lo que viví no fue positivo. Y llega un punto en el que tienes que probar algo nuevo, y es por eso que estoy aquí”.
También tuvo un trauma en su vida que nunca había enfrentado realmente. Cuando Downie tenía 8 años, su padre murió en un accidente automovilístico que lo llevó a practicar hockey. Lanzarse profundamente en el deporte fue su única forma de sobrellevar la muerte de su padre. Al igual que Cote, su compañero de equipo en los Flyers durante dos años, jugó de manera imprudente imprudente, lanzándose a colisiones violentas que lo dejaban a él y a sus oponentes ensangrentados.
Después de una carrera juvenil empañada por una controversia de novatos, Downie comenzó su primera temporada en la NHL, en 2007, con una suspensión de 20 juegos por un brutal control en las tablas en un competencia de pretemporada que envió a su oponente fuera del hielo en camilla.
Sigue siendo una de las suspensiones más largas jamás emitidas por la liga. En la prensa de hockey, fue etiquetado como un villano, un matón y un psicótico extremo. Las palabras le dolieron un poco, incluso cuando trató de reírse de ellas.
“No tengo dientes y soy pequeño, así que no pueden estar tan equivocados”, dijo Downie. “¿Bien? Al final del día, era un trabajo. Hice lo que me pidieron”.
Durante sus nueve temporadas jugando para cinco equipos de la NHL, sufrió más conmociones cerebrales de las que podía recordar. Sordo de un oído, al borde de las lágrimas todos los días y bastante seguro de que estaba bebiendo demasiado, Downie, que ahora tiene 36 años, se miraba en el espejo algunos días y se preguntaba si estaría muerto en seis meses.
No sabía nada sobre psicodélicos, solo que Cote le había dicho que lo ayudaría cuando Downie estuviera listo.
“Llamé a Riley y le dije: ‘Necesito algo, hombre’. Me cansé de ir a los médicos y hablar con ellos”, dijo Downie. “Muchas de las pastillas que te dan, te comen el cerebro. Realmente no te ayudan”.
Justin Renfrow, un jugador de línea de 33 años que jugó en la NFL y en Canadá, llegó en busca de claridad. Estaba considerando retirarse del fútbol profesional, algo que lo asustaba y lo emocionaba. Había estado jugando durante la mitad de su vida, y el juego era una gran parte de su identidad. Fue la última conexión que tuvo con su abuela, una de las personas más importantes de su vida. Ella fue la que iba a los viajes de reclutamiento con él. Después de su muerte en 2021, Renfrow sintió que una parte de ella todavía estaba con él mientras jugara.
Pero después de una década de jugar profesionalmente, el cuerpo de Renfrow estaba maltratado. Le dolía una de las rodillas. Había llegado a odiar las drogas farmacéuticas. Dijo que los médicos del equipo le habían recetado tantos medicamentos diferentes, incluidos los que cubren el estómago y los bloqueadores de los nervios para que pudiera tomar más analgésicos, que su cuerpo comenzó a experimentar terribles efectos secundarios.
Dijo que una vez tuvo una reacción tan mala a una combinación de analgésicos que le habían dado que necesitó atención médica después de sudar a través de su ropa y tener problemas para respirar.
“Es solo, ‘Necesitamos llegar a los playoffs, así que toma esto'”, dijo Renfrow. “Lanzó mi cuerpo en picada”.
Había usado hongos psicodélicos en numerosas ocasiones, principalmente como una forma de lidiar con el dolor provocado por el fútbol americano, pero nunca los había usado como parte de una ceremonia o para meditar. En este viaje, buscó claridad. ¿Era hora de alejarse del fútbol? Le apasionaba la cocina y estaba pensando en iniciar su propio programa en YouTube. Tal vez era hora de cambiar su enfoque y dejar que el fútbol se desvaneciera.
“Tengo muchas personas que dependen de mí todos los días”, dijo Renfrow.
Los atletas esperaban que la ceremonia los ayudara a obtener respuestas.
La investigación sobre psicodélicos es prometedora y emocionante, pero la efectividad de los hongos como tratamiento no está del todo establecida. Pero incluso si la psilocibina y otros psicodélicos resultan ser nada más que un placebo, lo que algunos investigadores dicen que es posible, muchos atletas juran que están encontrando un alivio real de la ansiedad, la depresión y otros traumas persistentes de sus días de juego.
Con un mercado global potencial multimillonario, también hay un gran incentivo financiero. Wake es solo una de un número creciente de nuevas empresas con fines de lucro respaldadas por dinero de inversión privada que buscan una parte del tratamiento psicodélico.
Eventualmente, ellos y otros esperan abrir centros de tratamiento o vender las drogas en los Estados Unidos y Canadá. En Canadá, la producción, venta o posesión de hongos psicodélicos son ilegales.
Durante el retiro de Jamaica, los líderes de Wake dieron una presentación a los participantes sobre cómo podrían invertir en la empresa.
Macleod dijo que se interesó en la terapia psicodélica no como una oportunidad comercial, sino después de que perdió a su hermana, Heather, hace seis años por suicidio.
Perderla lo llevó a buscar respuestas. Su hermana había sido esquiadora competitiva en Canadá, pero una serie de caídas le provocaron múltiples conmociones cerebrales y durante su vida adulta tuvo ansiedad y depresión. La medicina tradicional le falló repetidamente, dijo Macleod. Cada semana, se encuentra deseando haber sabido lo que sabe ahora y haberlo usado para intentar salvarla.
“No puedo decirte cuántas personas vienen a mí que están luchando como mi hermana”, dijo. “Dios, desearía que ella pudiera estar aquí. Sé que ella nos estaría animando. La veo a veces mirándonos desde arriba y diciendo: ‘Ayuda a otras personas que estaban atrapadas donde yo estaba'”.
Ansiosas por llevar los tratamientos psicodélicos a los consumidores, las empresas corporativas a menudo extrapolan los resultados de la investigación de ensayos clínicos estrictamente controlados con pacientes cuidadosamente seleccionados para promover un uso más amplio por parte de la población general en casi cualquier entorno.
“La presión por los psicodélicos generalmente está siendo impulsada por personas que quieren ganar dinero, mucho más que por científicos”, dijo Kevin Sabet, ex asesor principal de la Oficina de Política Nacional de Control de Drogas de la Casa Blanca, y ahora presidente y director ejecutivo de Smart Approaches to Marijuana, un grupo político que se opone a la legalización de la marihuana.
“¿Por qué dejaríamos que los inversionistas de Wall Street, que son realmente los que están aquí tratando de ganar dinero, lideren la conversación?”, agregó.
La comercialización podría ser tanto buena como mala para los psicodélicos. Por un lado, podría proporcionar financiación para la investigación; por otro, el deseo de rentabilizar esa inversión podría influir indebidamente en los resultados y poner en riesgo a los pacientes.
“Tu modelo de negocio no va a funcionar bien cuando alguien salta por la ventana y aparece en la portada de The New York Times”, dijo Johnson, el investigador de Johns Hopkins.
La investigación clínica también debe superar la imagen del hongo como una droga de fiesta, algo que los hippies comparten en bolsas de plástico en las últimas filas de los conciertos.
Para cambiar esa narrativa, dicen Wake y otras compañías, se están inclinando mucho hacia la ciencia. Esto no es una búsqueda de emociones, dicen, sino una medicina legítima que trata condiciones psiquiátricas reales.
Es el mismo argumento que hicieron los defensores de la legalización de la marihuana, ya sea que lo creyeran o lo estuvieran usando como un medio para un fin: presionar para legalizar el cannabis como medicina antes de abrir las puertas al uso recreativo sin restricciones.
Los líderes de Wake, como la mayoría de los ejecutivos en el universo psicodélico, han dicho que están comprometidos a ayudar en la investigación para demostrar a los reguladores federales que la psilocibina es segura y efectiva. Las muestras de sangre y saliva que recolectó un médico en el retiro de Wake, dijeron, se usarían para identificar marcadores genéticos que podrían predecir quién responderá al tratamiento con psilocibina.
El equipo de Wake hizo que los participantes usaran un casco que contenía tecnología de imágenes experimentales que se había utilizado en ensayos clínicos para rastrear la actividad cerebral antes, durante y después de las experiencias psicodélicas. Como parte de la investigación, los participantes usaron el casco mientras jugaban juegos de palabras.
Muchos investigadores académicos se preguntan si algunas empresas simplemente están aplicando un barniz de ciencia a un esfuerzo por hacer dinero, lo que muchos escépticos denominan “teatro placebo”.
De hecho, Aaronson teme que el campo pronto pueda estar “lleno de vendedores ambulantes”.
“El problema que tienes es que, como era de esperar, las redes sociales y las comunicaciones funcionan mucho más rápido que la ciencia”, dijo. “Entonces, todos están tratando de tener en sus manos estas cosas porque creen que será increíble”.
Aaronson ha diseñado protocolos de ensayos clínicos para Compass Pathways, una empresa competidora con fines de lucro que busca comercializar tratamientos con psilocibina, y ha rechazado a otras empresas que buscan crear una huella en el espacio psicodélico. (Aaronson recibe fondos de Compass para respaldar su investigación, pero dijo que no tiene ningún interés financiero directo en la empresa).
“Me preocupa quién respalda el juego de algunas de estas compañías y trato de averiguar qué es lo que realmente busca alguien”, dijo. “Hablas con la gente y ves si hay un plan real para investigar o si hay un plan real para vender algo”.
***
Un murmullo de tensión nerviosa perduraba en el aire mientras los atletas se preparaban para la ceremonia. En el desayuno, no hubo muchas conversaciones triviales. Los asistentes se arremolinaron y se registraron con el personal médico de Wake para ofrecer sus muestras de sangre y saliva. Algunos participaron en una clase de yoga en un estudio al aire libre con vista a la jungla.
Wake había contratado a una chamán jamaicana, una mujer llamada Sherece Cowan, una empresaria de comida vegana que fue finalista de Miss Universe Jamaica 2012, para dirigir a los atletas en la ceremonia. Pidió que la llamaran Sita y se refirió a sí misma como facilitadora de medicina natural.
Habló lenta y deliberadamente, agitando el humo de una urna mientras instaba a los participantes a reunirse en círculo en el césped de la finca. Después de beber una dosis de 3 a 5 gramos de psilocibina, que había sido molida en polvo y mezclada con jugo de naranja, los atletas cayeron en un estado de sueño durante las próximas cuatro a seis horas.
“Espero que obtengas todo lo que necesitas. Puede que no sea todo lo que estás pidiendo, pero espero que recibas todo lo que necesitas”, dijo Cowan. “Bendiciones en tu viaje”.
Un músico local comenzó a tocar, sus tambores y campanas pretendían realzar el viaje. La mayoría de los atletas yacían sobre colchonetas, como si durmieran. Cote se sentó en una pose de yoga. Nick Murray, director ejecutivo de Wake, le había pedido a Cote que usara un casco especial, un dispositivo de electroencefalografía más pequeño que el otro casco, para medir su actividad cerebral.
Excepto por los tambores y las campanas del músico, todo estaba en silencio. De vez en cuando, el viento agitaba las hojas de los árboles en el límite de la propiedad, pero durante las siguientes seis horas, dentro del círculo, el tiempo casi se detuvo.
Dos horas después de la ceremonia, después de que el psicodélico había hecho efecto, lo que estaba ocurriendo pasaba dentro de las cabezas de los atletas. Cote, sorprendentemente, seguía manteniendo su postura de yoga.
El silencio se rompió cuando Renfrow se levantó de su estera después de tres horas. Llevaba una sudadera en la ceremonia con sus iniciales, JR, estampadas en el pecho. Se quitó la camisa de su cuerpo con frustración y la arrojó a un lado.
Las lágrimas se derramaron por su rostro.
Cuando la ceremonia terminó, los atletas comenzaron a sentarse y algunos charlaron en voz baja.
La mayoría no estaba seguro de cómo describir la experiencia. Para algunos, se sintió como un descenso a los rincones de la mente, con colores y emociones mezclándose. Otros dijeron que enfrentaron traumas que pensaron que habían enterrado o emociones que querían reprimir. Dijeron sentir una conexión con las otras personas en el círculo.
“Es el último asesino del ego porque, al menos para mí, te da una empatía increíble que nunca antes habías sentido”, dijo Lee. “Cuando estás haciendo un viaje con otras personas, te ves a tí mismo en ellos. Es casi como si estuvieras caminando frente a un espejo, diferentes espejos. Ves partes de tí mismo en todos y te das cuenta de que todos estamos conectados y todos estamos pasando por algo, todos tenemos algún tipo de dolor, y eso te vuelve humilde”.
La mayoría de los atletas se quedaron solos para poder anotar sus pensamientos en un diario, siguiendo las instrucciones del personal de Wake. Habría una sesión de terapia comunitaria a la mañana siguiente.
A cada uno se le pediría que compartiera algo de su viaje.
***
Al final, la mayoría de los curiosos sobre la psilocibina simplemente quieren saber: ¿Funciona? Y, ¿cómo funciona? Los científicos dicen que esas son preguntas difíciles de responder en este momento.
Investigadores han descubierto que los psicodélicos clásicos, como la psilocibina y el LSD, actúan sobre el receptor de serotonina 2A, el mismo receptor al que se apuntan los antidepresivos más comunes del mercado. Pero más allá de eso, la comprensión de cómo funcionan para ayudar a las personas es, en este punto, más teoría o conjetura que hecho científico.
Johnson, el investigador de Johns Hopkins, dijo que la psilocibina ayuda a aumentar la apertura en las personas, permitiéndoles salir de su visión de quiénes son. Alguien que se resigna a ser un fumador que no puede dejar de fumar o una persona con depresión que no puede encontrar la felicidad puede, bajo la influencia de los psicodélicos, verse a sí mismo de una manera diferente, explicó.
“Una vez que están fuera de la trampa mental, se vuelve tan obvio para las personas con estos diferentes trastornos que, ‘¿Sabes qué? Puedo simplemente decidir dejar de fumar. Puedo dejar de lado mi tristeza’”, dijo Johnson.
Estudios con ratas muestran que los psicodélicos también parecen aumentar la conectividad neuronal en el cerebro, incluso después de una sola dosis. Eso podría ayudar al cerebro a recuperarse de lesiones traumáticas o conmociones cerebrales, encontrando nuevos caminos alrededor de las áreas dañadas.
La teoría predominante de cómo la psilocibina y otros psicodélicos podrían ayudar a tratar la salud mental es que reprimen la actividad en la red de modo predeterminado del cerebro. Es un conjunto de regiones del cerebro que se activan cuando las personas reflexionan sobre algo, y una de las pocas partes que está hiperactiva en las personas con depresión.
A menudo revisan los errores que cometieron una y otra vez o se castigan continuamente por ellos, dijo LaPratt, el investigador de Sheppard Pratt. Esa hiperactividad en la red de modo predeterminado conduce a patrones repetitivos de pensamientos negativos. ¿Qué me pasa? ¿Por qué soy tan infeliz? De los cuales la persona no puede escapar.
Las personas con depresión suelen reflexionar sobre el pasado; personas con ansiedad, sobre el futuro.
“Es posible que surja algo y luego el cerebro comience a pensar, y nuevamente, como ese disco rayado”, dijo LaPratt. “Puede ser muy fácil comenzar a pensar en cómo todo podría salir mal y comenzar a dramatizar”.
Ese pensamiento repetitivo también prevalece en personas con otras afecciones, incluido el trastorno obsesivo compulsivo y el trastorno por estrés postraumático. Comienza a afectar el sentido de quiénes son; se definen a sí mismos por su condición.
Pero los psicodélicos parecen ayudar a las personas a examinar viejos traumas sin volver a caer en el mismo ciclo destructivo. Pueden ayudar a las personas a sentirse más conectadas con los demás. La depresión y la ansiedad no se borran simplemente, dijo LaPratt, sino que las personas pueden obtener una nueva perspectiva de sus problemas y comenzar a sentir, tal vez por primera vez, que pueden deshacerse de ellos.
“Vemos una mayor apertura y cierta motivación para cambiar los comportamientos”, dijo.
La mayoría de los psicodélicos están fuera del sistema de una persona a la mañana siguiente, pero, según los investigadores, esa mayor apertura puede durar semanas o meses sin dosis adicionales, lo que brinda una ventana durante la cual pueden comenzar a abordar sus problemas.
“Quizás estemos ayudando a las personas a llegar al punto de poder aceptar las cosas que no pueden cambiar y cambiar las cosas que sí pueden”, dijo Aaronson, haciéndose eco de la Oración de la serenidad, que a menudo se usa en los ejercicios de 12 pasos de los programas de recuperación. “Se les quita autonomía personal a las personas con depresión. No sienten que puedan operar en su mejor interés. Se ven atrapados en un conflicto interno. Y creo que esto les ayuda a ir más allá de eso”.
Por la mañana, los atletas se reunieron en un patio para una forma de terapia de grupo llamada integración. Estaba previsto que durara al menos dos horas. Macleod explicó que era una parte esencial para comprender el viaje de la psilocibina. Todos los asistentes tuvieron la oportunidad de compartir algo de su experiencia, ya fuera esclarecedor, confuso, edificante o una mezcla de muchas emociones.
Lee habló sobre su ansiedad, sobre tratar de entender cuál sería su identidad ahora que no era boxeador. Al alejarse del ring, temía estar decepcionando a todas las personas que lo apoyaron cuando eligió una carrera de boxeo en lugar de un trabajo en finanzas después de graduarse de Notre Dame.
Pero ahora había llegado a comprender que esas eran sus propias inseguridades. Podía seguir su propio camino. Podría ayudar a las personas que experimentan un dolor físico y emocional similar.
Renfrow respiró hondo varias veces mientras buscaba las palabras. Durante la mayor parte de su vida, se había visto a sí mismo como un jugador de fútbol americano. Pero en su viaje de psilocibina, sintió como si los miembros de su familia le dijeran que estaba bien dejarlo ir. Cuando se puso de pie durante la ceremonia y se quitó la camisa con sus iniciales, dijo que, simbólicamente, estaba soltando algo.
“Está bien dejar de perseguir el viaje del fútbol”, dijo Renfrow. “No voy a vestirme bien este año y eso está bien para mí. Seré capaz de resolverlo.
Al decir adiós al fútbol, dijo, se estaba despidiendo de su abuela.
“El fútbol era ella”, dijo Renfrow, y comenzó a llorar. “Fuimos a todos mis viajes de reclutamiento. Así que tuve que dejarla ir dejando ir al fútbol. Y ese fue un gran momento cuando me puse de pie. Tuve que dejarla ir. Así que fue difícil, pero tenía que hacerlo”.
Cuando fue el turno de Downie, trató de calmar la tensión bromeando, diciendo que era hora de ir a comer. No quería abrirse al grupo, dijo. Había escrito algunas notas en una hoja de papel. Sus manos temblaban mientras trataba de leerlas.
“No estaba bebiendo y no estaba consumiendo drogas por diversión”, dijo Downie con voz temblorosa. “Estaba adormeciendo mi cerebro porque estaba jodido. No pude salir de mi camino de entrada durante un año. Me senté en cuartos oscuros y recurrí a las drogas y el alcohol”.
Pero dijo que en el viaje psicodélico pudo conectarse con su pasado. “Estoy sentado allí y estoy repasando mi cerebro, estoy hablando con mi papá, estoy hablando con los miembros de mi familia. He pedido perdón a todos los que podría pedir perdón”, dijo. “Me hizo llorar. Me hizo sentir bien”.
Se dio cuenta, a través del viaje, que quería ser un mejor hombre. Su voz temblaba mientras trataba de pronunciar las palabras.
“Al final de todo esto, creo que lo que he aprendido es cómo controlar lo que sucede. yo tengo el control. Puedo controlar esto”, dijo. “Me iré a casa y me identificaré y ejecutaré y seré un mejor padre y me quedaré para mis hijos, lidiaré con mis conmociones cerebrales lo mejor que pueda”.
Se giró para mirar directamente a Cote, las lágrimas corrían por sus mejillas detrás de sus gafas de sol.
“Quiero decir esto, hermano, cuando digo que me salvaste la vida”.
Cuando las palabras de Downie dieron paso al silencio, Lee se levantó de su silla. Cruzó el círculo, se acercó a Downie y abrió los brazos. Los dos luchadores, que llegaron a Jamaica tristes y destrozados, se abrazaron.
***
Si bien los estudios han encontrado que la psilocibina junto con la terapia es más efectiva que la terapia sola, no está claro si la psilocibina sola, sin el trabajo preparatorio o la integración posterior, tiene algún efecto.
“Hay una razón por la cual las personas que van a raves y toman psilocibina no se curan”, dijo Aaronson. “La psilocibina no es un antidepresivo”.
Incluso dentro de los estrictos protocolos de ensayos clínicos, la pregunta sigue siendo si la terapia asistida por psilocibina funciona. Los estudios preliminares han sido prometedores, pero el número de sujetos de prueba ha sido pequeño. Se necesitan estudios mucho más amplios para determinar tanto la seguridad como la eficacia.
Aún así, eso no ha impedido que los defensores de la psilocibina promocionen la investigación hasta la fecha, lo que implica que es más definitiva de lo que es. Además, muchos evangelistas de los hongos atribuyen los efectos positivos de los ensayos clínicos al consumo de psilocibina en general, descartando los protocolos utilizados en los estudios.
En el retiro de Wake en Jamaica, por ejemplo, los atletas tomaron psilocibina en ceremonias grupales guiadas por Cowan, la chamán local, mientras que las sesiones de integración grupal fueron dirigidas por un médico osteópata. Ninguno de los dos era un psicoterapeuta autorizado, dijo Murray. No está claro si los beneficios de la terapia con psilocibina sugeridos por la investigación clínica se aplicarían a un entorno grupal, para la dosificación o la integración.
Murray, director ejecutivo de Wake, dijo que si bien la investigación clínica se esfuerza por eliminar cualquier variable, como las interacciones entre los participantes, los líderes de Wake sienten que el entorno grupal ofrece beneficios a sus clientes.
“Es ese grupo que siente que, ‘Estamos juntos en esto. Mi divorcio es como tu divorcio. Perdí a un hermano’”, dijo. “Eso es difícil de poner en un ensayo clínico”.
Wake se había registrado para realizar un ensayo clínico en Jamaica, pero Murray dijo que la compañía finalmente decidió no continuar, centrándose, en cambio, en ofrecer tratamiento.
Aún así, Murray dijo que Wake está contribuyendo a la investigación científica: recolectaron muestras de sangre y saliva, y se les pidió a los participantes que completaran cuestionarios antes y después del retiro para ayudar a evaluar si el tratamiento había funcionado.
Murray dijo que Wake usa los mismos cuestionarios validados clínicamente que se usan en el consultorio de un psiquiatra.
“Entonces, no es teatro. Estas son las herramientas reales que se utilizan”, dijo. Sin embargo, sería difícil con el enfoque de Wake analizar si los hongos y la integración ayudaron a los participantes u otras influencias, como estar de vacaciones en Jamaica, estar entre un grupo de compañeros de apoyo o la marihuana que muchos de ellos fumaban regularmente durante el retiro.
“Al menos tienes que escuchar y tomarlo en serio. Hay anécdotas de personas que dicen que se habrían suicidado”, dijo Johnson. “A veces ves solo la experiencia de ‘full monty’, donde esta persona está allí en una trayectoria oscura, oscura y toda su vida cambia. Sospecho que esto es real. Algo está pasando con estos atletas que hacen estos informes”.
Las anécdotas brillantes, particularmente cuando provienen de atletas o celebridades de alto perfil, tienen peso entre el público y ayudan a impulsar medidas como las de Oregon y Colorado que están estableciendo vías para el tratamiento con psilocibina, independientemente de lo que piensen los investigadores o los reguladores.
“Cuando las personas están molestas y no satisfacemos sus necesidades, van a probar cosas”, dijo Atheir Abbas, profesor asistente de neurociencia del comportamiento en la Oregon Health & Science University. “Con suerte, los científicos pueden ponerse al día para comprender por qué las personas piensan que esto es realmente útil. Y tal vez sea útil, pero tratemos de averiguar si lo es y cómo”.
Pero existe el peligro de tomar estas historias, sin importar cuán convincentes sean, y extrapolar su seguridad o eficacia.
“La parte difícil es que el plural de anécdota no son datos”, dijo Sabet, el CEO de Smart Approaches to Marijuana. “Y los datos aún no están allí”.
***
Un año después del retiro, Downie, Renfrow y Lee dijeron que creían que su viaje con la psilocibina los había ayudado. No solucionó mágicamente todos sus problemas, pero cada uno lo consideró una experiencia positiva.
Downie ya no siente que está atrapado en un lugar oscuro. Dijo que cuando regresó a Ontario, su familia notó una diferencia de inmediato.
“Ese viaje me dio mucha claridad”, dijo Downie. “Te da direcciones. Te da respuestas internamente. Es algo único que experimenté. Mi año fue definitivamente mejor que el año anterior, eso es seguro… ¿Creo que podría ayudar a otras personas? Yo diría que sí. ¿Me ayudó? Absolutamente”.
Sin sentirse más como un prisionero en su casa, Downie comenzó un campamento de motos de nieve que lleva a los adultos en aventuras guiadas por Moosonee, cerca de James Bay. Es algo que solía hacer con su familia antes de que despegara su carrera en el hockey.
“No es mucho de lo que presumir, pero es lo más al norte al que puedes ir en una moto de nieve en Ontario”, dijo Downie. “Vienen muchos adultos de todas partes. Es una experiencia genial. Siempre ha sido una de mis pasiones”.
Todavía tiene problemas persistentes por sus conmociones cerebrales y sospecha que siempre los tendrá.
“Es lo que es”, dijo. “¿Diría que está mejorando? Es un proceso”.
El resultado más positivo ha sido la alegría que ha encontrado en ser padre.
“Mi pequeño está empezando a enamorarse del hockey, que es algo que he estado esperando”, dijo Downie.
Aunque Downie no ha realizado otro viaje con psilocibina, dijo que estaría abierto a hacerlo.
Renfrow salió de la ceremonia con la intención de retirarse del fútbol profesional, pero tres meses después volvió a firmar con Edmonton Elks de la Canadian Football League. Este año, se unió a los Jacksonville Sharks de la National Arena League, en parte para estar más cerca de su hijo.
“En ese momento, pensé que iba a dejar el fútbol”, dijo.
Pero se siente cómodo donde está y dice que está cumpliendo sus objetivos, incluido presentar ese programa de cocina en YouTube que esperaba hacer. Y dijo que se está divirtiendo de nuevo. Ahora recurre a los hongos cada vez que tiene que tomar una gran decisión.
“Creo de todo corazón en eso y en todo el tipo de orientación que me ha dado”, dijo. “No podrías pedir algo mejor, haber seguido la guía de un viaje con hongos”.
Lee se mudó de California a Austin, Texas, y ahora dirige un negocio de CBD con su hermana. Encontrar su identidad posterior al boxeo sigue siendo un proceso. En sus viajes psicodélicos en el retiro de Wake, dijo Lee, nunca pensó en deportes o boxeo. Sus visiones eran todas sobre la familia, Dios, el universo.
“Simplemente me hace darme cuenta de la importancia que le estoy dando a algo que a mi subconsciente ni siquiera le importa”, dijo. “A mi subconsciente no le importa que sea boxeador, que fui luchador e hice esto y aquello. Es todo tipo de ego”.
La experiencia, dijo, lo ayudó a comprender cuán poderosa puede ser la mente, que puede ser un amigo o un enemigo.
“Salí de eso dándome cuenta de que tengo todas las herramientas para curarme a mí mismo”, dijo. “Eso es enorme. Porque, especialmente para los muchachos que han tenido conmociones cerebrales o atletas o lo que sea, te sientes un poco aislado, te sientes solo, te sientes sin esperanza. Así que te da un sentido de esperanza”.
Le permitió ir más allá de la necesidad de probarse a sí mismo, en el ring o fuera de él, para dejar de medir su valor por sus logros. Se ha obsesionado con actividades mucho más tranquilas y no violentas: el surf y el pickleball.
“Puedo apagar mi cerebro como en el boxeo”, dijo. “Pero al mismo tiempo, es más fácil para mi cuerpo y simplemente, no sé, más satisfactorio. No tengo que probar nada”.
El viaje a Jamaica le está permitiendo salir adelante, hacer el trabajo necesario para sanar.
“Una parte de mí entró con la esperanza de que todos mis problemas se resolvieran, pero poner esas expectativas puede ser difícil”, dijo. “¿Estoy curado? No. ¿Pero realmente ayudó? ¿Y fue como una de las experiencias más profundas de mi vida?
“Yo diría que sí”.
Este artículo fue producido y escrito por Markian Hawryluk de KFF Health News y Kevin Van Valkenburg de ESPN. El investigador John Mastroberardino colaboró con la historia.
Si tu mismo o alguien que conoces puede estar experimentando una crisis de salud mental, llama o envía un mensaje de texto a la Línea de vida de crisis y suicidio al 988 o a la Línea de texto de crisis enviando un mensaje de texto con “HOME” al 741741. En Canadá, llama a Talk Suicide Canada al 1-833- 456-4566 o envía un mensaje de texto al 45645 de 4 pm a medianoche ET.
[Nota del editor: como parte del reportaje de este artículo, algunos miembros del equipo de reporteros de ESPN, bajo la guía del personal de Wake Network, usaron psilocibina. Wake Network fue compensado, pero no por ESPN.]
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
2 years 3 months ago
Health Industry, Mental Health, Noticias En Español, Pharmaceuticals, States, Colorado, Oregon, texas
Pain, Hope, and Science Collide as Athletes Turn to Magic Mushrooms
If you or someone you know may be experiencing a mental health crisis, call or text the 988 Suicide & Crisis Lifeline at 988 or the Crisis Text Line by texting “HOME” to 741741. In Canada, call Talk Suicide Canada at 1-833-456-4566 or text 45645 from 4 p.m.-midnight ET.
WAKEFIELD, Jamaica — The boxer felt broken. Every day, he was waking up in pain. Some days, it was debilitating headaches. Other times, it was his back. Or his fists. His ribs. His nose. On top of that, he had mood swings. Depression. Anxiety.
Mike Lee didn’t regret his career. He had been one of the best professional fighters in the world in his weight class. He’d gone 21-1 professionally and fought in Madison Square Garden and in front of millions on TV.
But it had been more than two years since he’d been inside a ring, and every day was a reminder of the cost. At one point, Lee was taking eight prescription medications, all of them trying to help him cope. In his lowest moment, on a night when he was in the depths of an addiction to painkillers, he said, he contemplated driving his car into the median of a Chicago freeway at 140 mph. He was willing to do anything to escape the hell he felt trapped in.
The impulse faded, but the pain remained.
He was lost.
“When you’re in pain and you’re stuck in a corner, you’ll do anything to get out of it,” Lee said.
Now, he had come to a verdant jungle at the end of a dirt road halfway up a mountain.
Psychedelic mushrooms, he hoped, could change his life.
Lee was part of a small group — many of them retired athletes — who’d traveled to Jamaica in March 2022 for a retreat costing as much as $5,500. They each had come to the Good Hope Estate, a sugar plantation turned exclusive resort, hoping to rid themselves of depression, anxiety, and chronic pain they had experienced for years.
Two psychedelic mushroom ceremonies and two therapy sessions awaited them at the retreat run by a Canadian company called Wake Network. The participants were nervous, but also hopeful.
Along with Lee, there was a professional football player considering retirement and a former hockey star who had multiple concussions. They’d come from all over North America, from different backgrounds and different sports, but they had a few things in common: They were vulnerable, and they felt that prescription medications had failed them. They didn’t know what to expect, whether the treatment would work, whether they’d return home with a solution or just more disappointment.
Lee had learned about the retreat from a childhood friend who works as a doctor for Wake. Others had been recruited by Riley Cote, a former enforcer with the Philadelphia Flyers and now a psychedelics evangelist who is an adviser to Wake with an equity stake.
Cote was once just like Lee. He used to love punching people in the face. He loved the way his hand landed with a thud when his knuckles connected with flesh and bone at a violent speed. Snapping someone’s head back made Cote feel alive.
“I fought everyone and their brother in my career,” Cote said. “I would pick out the biggest guy I could find and challenge him. It was how I survived, how I made a name for myself. I was inflicting all this pain and inflammation on myself, always getting punched in the face, and I had to keep up with this macho type of personality, like, ‘Oh, you can’t hurt me. You can’t hurt me.’”
He was no longer that person. It made him cringe to think about the man he once was, someone who drank excessively and used painkillers to numb his brain. There was a time when he, like Lee, was in a dark place, but over the course of several years, psychedelic mushrooms, Cote believes, helped bring him back into the light.
“The world is in a crisis, a mental health crisis, a spiritual crisis,” Cote said. “And I think these are spiritual medicines, and I just feel like it’s the right path for me. I don’t think of it as anything more than my duty, my purpose on this planet is to be sharing the truth around natural medicine.”
For years, whispers have circulated about an underground network of athletes — primarily ex-athletes — using psilocybin, the compound in magic mushrooms, to treat traumatic brain injuries, anxiety, and depression. Many of them, like Cote, view psychedelics as a miracle cure, the one thing they’d been able to find that could help break a cycle of pharmaceutical painkillers and substance abuse. They gathered in small groups to ingest mushrooms in private or traveled to countries such as Jamaica where psychedelic mushrooms aren’t prohibited.
Now the use of psychedelic mushrooms is gaining traction in the United States. A number of cities have decriminalized possession of psilocybin, and Oregon and Colorado voters passed ballot measures to legalize magic mushrooms under supervised use. Many researchers predict FDA approval of a psychedelic treatment will come within the next five years.
But many of those same researchers warn the hype over psychedelics is outpacing the science — and that the treatment comes with significant risks for some patients. They fear that, unless research is conducted methodically and ethically, widespread use of psilocybin could result in a public backlash, as it did in the 1960s, relegating a promising treatment to the dustheap of banned substances.
They are urging corporate entities like Wake, which are already positioning themselves to take advantage of the potential legalization of psychedelics, to go slowly, ensure the research is done the right way, and allow the science to catch up.
“If you don’t do this safely, people are going to get hurt,” said Matthew Johnson, a psychiatry professor and psychedelics researcher at Johns Hopkins University.
But many — including former pro athletes with battered bodies and brains — don’t want to wait for the slow grind of clinical research. They need help now. The painkillers, the antidepressants, the countless different pills they were prescribed over the years haven’t helped. In their minds, the stories told by fellow athletes who say they have benefited from psychedelics outweigh any scientific uncertainty.
“When you think of magic mushrooms, you think of hippies at Woodstock dancing around to music,” Lee said. “To think about you’ve got some of the best athletes in the world here that are dealing with some stuff and they’re taking it, it makes you feel more comfortable. It makes me feel like, ‘OK, maybe I’m doing the right thing.’ It’s a healing medicine; it’s not just a party drug.”
***
Cote, now 41, was a decent hockey skater growing up in Winnipeg, Manitoba, tenacious as hell from end to end and a tireless worker, but fairly average at handling the puck. He didn’t score enough goals to rise through junior hockey the way some prospects did. Yet as he got older, coaches didn’t mind as much. He had broad shoulders and a long reach. In an era of hockey where violence was still currency, he had found his golden ticket to the NHL: Cote would beat on people and get beat on in return. As a member of the Flyers, he saw it as his duty to uphold the traditions of the Broad Street Bullies, a group of players from the 1970s who were celebrated by the press for playing — and partying — hard.
He fought his way through the NHL for portions of four seasons, accumulating more than 400 career penalty minutes while scoring just one goal. Most of his fights were brutal, barbaric affairs. His highlight reel shows a hulking giant, his eyes filled with violence, the kind of goon who could break your jaw and laugh maniacally in the aftermath, blood dripping from his face down onto the ice.
“It was something I enjoyed doing, and I think it was just an element of competition for me,” Cote said. “And it was also probably something I was doing out of fear — fear of not living my childhood dream or letting my parents down or people down.”
He said he medicated his pain nearly every day with booze. Beers were an appetizer on the way to doing shots at the bar. Shots often led to harder drugs. He and his teammates would stay out until 3 a.m., sometimes later, then try to sweat out the poison the next day during practice.
After a few years, his brain started to fog. He got bigger and stronger through weightlifting, and he looked like a monster on the ice, but every hockey skill except his fighting deteriorated. As his career wound down, he said, it felt as if darkness was creeping in. He grew depressed. He was afraid of what he’d become.
Today, Cote bears little resemblance to that enforcer in the videos. Thinner and calmer, he teaches yoga classes in a Delaware studio three times a week. With shoulder-length hair, tattoos on his arms and chest, he speaks with a soft baritone voice. He seems more monk than monster.
“I look back and it just shows maybe how confused I was and what reality I was seeking, which was supposedly happiness and fulfillment within chasing my childhood dream,” Cote said. “But it’s hard for me to wrap my head around me doing that now, just knowing who I am now, and realizing it takes a lot of darkness to do what I did.”
Cote said he took mushrooms recreationally throughout his 20s, but never in a therapeutic setting or with the understanding they might help him process both his physical and emotional trauma. “It was just part of the scene or part of the party,” he said.
But when he retired in 2010, he felt like he was facing an identity crisis. He had been a fighter for so long, he thought that’s all he was. How could a washed-up enforcer raise two daughters?
He started reading. What he learned shocked him.
Researchers had quietly revived the study of psychedelics as a medical treatment in 2000, and early findings suggested psilocybin often had noticeable benefits for people diagnosed with anxiety and depression. It helped some patients shed their addictions to drugs or alcohol. Other research suggested that psilocybin may actually be capable of reshaping the anatomy of the brain, restoring neuropathways, and helping heal traumatic brain injuries.
For Cote, who was diagnosed with at least three concussions in his hockey career and probably incurred many more, it was transformative.
Cote now recruits clients for Wake, which hosts immersive psilocybin retreats outside the U.S.
“Some people come to these events and they’re borderline suicidal,” said Tyler Macleod, a Wake co-founder and its chief experience officer. “They’re not fixed after one ceremony, but they’re not stuck in the dark anymore. They wake up and they’re like, ‘Oh, I can navigate a relationship with my kids again.’”
The ex-athletes who attend these retreats are all struggling with something, Cote said. They need help. In many cases, they feel as if they have tried everything else. He asks why they need to wait when so many studies and anecdotes indicate positive results?
“It’s like with cannabis: How many stories did we have to be told before we had a medical program?” Cote said. “It’s just been roadblocked for so long.”
***
In 1970, President Richard Nixon signed into law the Controlled Substances Act, legislation that divided drugs into five levels, ranking them based largely on their potential for abuse. Magic mushrooms were categorized as Schedule 1 substances, alongside heroin and marijuana, meaning the government believed they had no medical benefit as well as high potential for abuse. (Cocaine, oxycodone, and methamphetamine were all classified as Schedule 2 drugs.)
Those decisions — which Nixon adviser John Ehrlichman later said were politically motivated — continue to have a ripple effect today. Research into psychedelic treatments was put on hold for 30 years.
While the recent studies have been small in scope, they have shown remarkable effects. Prescription drugs approved for conditions such as anxiety or depression help at best 40% to 60% of patients. In early trials, psychedelics have reached efficacy rates of more than 70%.
And unlike most prescribed medications, which stop working soon after patients quit taking them, one or two treatments of psilocybin can have lasting effects of six months, a year, or even longer, according to one Johns Hopkins study. With minimal risk of addiction or overdose and centuries of use by Indigenous cultures, psilocybin is seen by many researchers as a potential breakthrough treatment with great benefits and few risks.
Scott Aaronson, director of clinical research programs at Sheppard Pratt, a nonprofit psychiatric hospital outside Baltimore, has been studying difficult-to-treat mood disorders for 40 years, starting with some of the early studies on Prozac.
“I’m a cynical, skeptical, sarcastic human being,” Aaronson said. “And I will tell you, I have never seen anything like it in all my years.”
But psilocybin is not without risks. It can exacerbate heart problems and trigger schizophrenia in those with a genetic predisposition, and the combination of psilocybin and lithium may cause seizures. Clinical trials have generally screened out patients at risk for such complications. Still, a significant portion of those who consume psilocybin, even without any of those concerns, have a negative experience.
“At a high dose, about a third of people in our studies, even under these ideal conditions, can have what would be called a bad trip, some degree of substantial anxiety or fear,” said Johnson, the Johns Hopkins researcher. “A person can be very psychologically vulnerable. It can feel like they’re dying.”
Sometimes, though, even those “bad trips” can lead to help with depression or other issues, researchers have found, especially with follow-up help from a therapist to process the experience.
The psychedelic effects of psilocybin can also disconnect a person from reality, which can lead people to do dangerous things, like running out into traffic or jumping out a window.
“The very conception of reality and themselves in reality, like who they are — these things can be profoundly changed and it’s not a good recipe for interacting in public,” Johnson said.
Researchers also describe cases where psilocybin puts people with unresolved psychological issues into long-term distress.
That’s why researchers are adamant that psilocybin should be administered in a clinical setting with trained therapists who can guide people through the experience, deal with negative outcomes when they emerge, and help people process and integrate their experiences.
Clinical trials of psilocybin have relied on strict protocols, involving one or more sessions before the treatment to help the test subjects understand what to expect. The ingestion of the mushrooms is often done in a single day, with one or two therapists on hand. In the following days, the person returns for what’s known as integration, typically a one-on-one therapy session to help process the experience and to begin the journey toward healing. Some trials add an extra day of therapy in between two treatments.
Unlike with a typical medication, patients aren’t sent home with a bottle of pills.The entire protocol is more like a medical procedure.
But it’s a misconception that it’s the psychedelic medicine doing all the work, not the therapy that comes afterward, said Jeffrey LaPratt, a psychologist and psilocybin researcher with Sheppard Pratt. “It’s really hard work and it takes vulnerability. It takes courage. It can be really painful.”
***
Former NHL player Steve Downie felt as if something in him was broken when he was invited to the Wake retreat in Jamaica. His days were filled with fog. He was living with depression, often unable to leave his home.
“I got tired of going to those doctors and tired of talking to them,” Downie said. “Don’t get me wrong — I’m not saying doctors are bad. I’m just saying, in my personal experience, what I went through, it wasn’t positive. And it just comes to a point where you got to try something new, and that’s why I’m here.”
He also had trauma in his life he’d never truly confronted. When Downie was 8 years old, his father died in a car crash driving him to hockey practice. Throwing himself deep into the sport was his only way of coping with his father’s death. Like Cote, his teammate on the Flyers for two years, he played the game with reckless abandon, launching himself into violent collisions that left both him and his opponents bloodied.
After a junior career marred by a hazing controversy, Downie started his first NHL season, in 2007, with a 20-game suspension for a brutal check into the boards in a preseason contest that sent his opponent off the ice on a stretcher. It remains one of the longest suspensions ever issued by the league. In the hockey press, he was labeled a villain, a thug, a goon, and borderline psychotic. The words stung a little, even when he tried to laugh them off.
“I got no teeth, and I am small, so they can’t be all that wrong,” Downie said. “Right? End of the day, it was a job. I did what I was asked.”
Over his nine seasons playing for five NHL teams, he endured more concussions than he could remember. Deaf in one ear, on the verge of tears every day, and fairly certain he was drinking too much, Downie, now 36, would look in the mirror some days and wonder if he would be dead in six months. He didn’t know anything about psychedelics, just that Cote had told him he would help when Downie was ready.
“I called Riley and I said, ‘I need something, man.’ I got tired of going to doctors and talking to them,” Downie said. “A lot of the pills they give you, they eat at your brain. They don’t really help you.”
Justin Renfrow, a 33-year-old lineman who played in the NFL and in Canada, came seeking clarity. He was considering retiring from professional football, something that both scared and excited him. He’d been playing for half his life, and the game was a huge part of his identity. It was the last connection he had to his grandmother, one of the most important people in his life. She was the one who went on recruiting trips with him. After she died in 2021, Renfrow felt that a part of her was still with him as long as he played the game.
But after a decade of playing professionally, Renfrow’s body was battered. One of his knees was aching. He had come to loathe pharmaceutical drugs. He said he’d been prescribed so many different drugs by team doctors — including stomach coaters and nerve blockers so he could take more painkillers — that his body started to experience terrible side effects. Once, he said, he had such a bad reaction to a combination of painkillers he’d been given, he needed medical attention after he sweated through his clothes and began to have trouble breathing.
“It’s just, ‘We need to make the playoffs, so take this,’” Renfrow said. “It threw my body into a tailspin.”
He’d used psychedelic mushrooms numerous times, mainly as a way to cope with the pain brought on by football, but he’d never used them as part of a ceremony or to be meditative. On this trip, he sought clarity. Was it time to walk away from football? He was passionate about cooking and thinking of starting his own show on YouTube. Maybe it was time to shift his focus and let football fade away.
“I’ve got a lot of people who depend on me every day,” Renfrow said.
The ceremony, the athletes hoped, would guide them toward some answers.
***
The research into psychedelics is promising and exciting, but the effectiveness of mushrooms as a treatment isn’t fully settled. But even if psilocybin and other psychedelics prove to be nothing more than a placebo — which some researchers say is possible — many athletes swear they are finding real relief from the anxiety, depression, and other traumas lingering from their playing days.
With a potential multibillion-dollar global market, there’s also a huge financial incentive. Wake is just one of a growing number of for-profit startups backed by private investment money staking a claim in the psychedelic treatment space. They and others hope to open treatment centers or sell the drugs in the U.S. and Canada eventually. Magic mushrooms are illegal to produce, sell, or possess in Canada.
During the Jamaica retreat, Wake leaders gave a presentation to participants on how they could invest in the company.
Macleod said he grew interested in psychedelic therapy not as a business opportunity but after he lost his sister, Heather, six years ago to suicide. Losing her drove him to search for answers. His sister had been a competitive skier in Canada, but a series of falls led to multiple concussions, and throughout her adult life she had anxiety and depression. Traditional medicine repeatedly failed her, Macleod said. Every week, he finds himself wishing he’d known then what he knows now and used it to try to save her.
“I can’t tell you how many people come to me who are struggling like my sister was,” he said. “God, I wish she could be here. I know that she’d be cheering us on. I see her sometimes looking down on us and saying, ‘Help other people who were stuck where I was.’”
Eager to bring psychedelic treatments to consumers, corporate firms often extrapolate research findings from tightly controlled clinical trials with carefully selected patients to promote broader use by the general population in almost any setting.
“The push for psychedelics generally is being driven by people that want to make money, much more than it is about scientists,” said Kevin Sabet, a former White House Office of National Drug Control Policy senior adviser who’s now president and CEO of Smart Approaches to Marijuana, a political group opposed to marijuana legalization. “Why would we let the Wall Street investors, who are really the ones here trying to make money, be driving the conversation?”
Commercialization could be both good and bad for psychedelics. On the one hand, it could provide funding for research; on the other, the desire for a return on that investment could improperly influence the results and put patients at risk.
“Your business model isn’t going to work well when someone’s jumped out of a window and it’s on the front page of The New York Times,” said Johnson, the Johns Hopkins researcher.
Clinical research must also overcome the mushroom’s image as a party drug, something hippies share out of plastic baggies in the back rows of concerts. To change that narrative, Wake and other companies say, they are leaning hard into the science. This isn’t thrill-seeking, they say, but legitimate medicine treating real psychiatric conditions. It’s the same argument proponents of marijuana legalization made, whether they believed it or were using it as a means to an end — pushing to legalize cannabis as medicine before opening the floodgates to unfettered recreational use.
Wake leaders, like most executives in the psychedelic space, have said they are committed to assisting research to prove to federal regulators that psilocybin is safe and effective. Blood and saliva samples a doctor collected at the Wake retreat, they said, would be used to identify genetic markers that could predict who will respond to psilocybin treatment.
Wake’s team had participants use a helmet containing experimental imaging technology that had been used in clinical trials to track brain activity before, during, and after psychedelic experiences. As part of the research, participants wore the helmet while playing games of Wordle.
Many academic researchers wonder whether some companies are simply applying a veneer of science to a moneymaking endeavor, what many skeptics refer to as “placebo theater.”
Indeed, Aaronson fears the field could soon be “full of hucksters.”
“The problem you’ve got is that, not surprisingly, social media and communications works much faster than science does,” he said. “So everybody’s trying to get their hands on this stuff because they think it’s going to be incredible.”
Aaronson has designed clinical trial protocols for Compass Pathways, a competing for-profit company seeking to market psilocybin treatments, and has turned down other firms looking to create a footprint in the psychedelic space. (Aaronson receives funding from Compass to support his research but said he has no direct financial interest in the company.)
“I worry about who’s backing the play from some of these companies and try to figure out what somebody is really after,” he said. “You talk to people and you see whether there’s a real plan to do research or there’s a real plan to sell something.”
***
A hum of nervous tension lingered in the air as the athletes prepared for the ceremony. At breakfast, there wasn’t a lot of small talk. The attendees milled about, checking in with Wake’s medical personnel to offer up their blood and saliva samples. Some participated in a yoga class in an outdoor studio that overlooked the jungle.
Wake had hired a Jamaican shaman — a woman named Sherece Cowan, a vegan food entrepreneur who was a 2012 Miss Universe Jamaica runner-up — to lead the athletes in the ceremony. She asked to be called Sita and referred to herself as a plant medicine facilitator.
She spoke slowly and deliberately, waving smoke from an urn as she urged participants to gather in a circle on the lawn of the estate. After drinking a 3- to 5-gram dose of psilocybin, which had been ground into a powder and mixed with orange juice, the athletes would slip into a dream state for the next four to six hours.
“I hope that you get all that you need. It may not be all that you’re asking for, but I hope you receive all that you need,” Cowan said. “Blessings on your journey.”
A local musician began to play, his drums and chimes intended to enhance the journey. Most of the athletes lay on mats, as if sleeping. Cote sat in a yoga pose. Nick Murray, Wake’s CEO, had asked Cote to wear special headgear — an electroencephalography device smaller than the other helmet — to measure his brain activity. Except for the musician’s drums and chimes, it was quiet. The wind occasionally rustled the leaves on the trees at the edge of the property, but for the next six hours, inside the circle, time mostly stood still.
Two hours into the ceremony, after the psychedelic had kicked in, whatever was taking place was occurring inside the athletes’ heads. Cote, remarkably, was still holding his yoga pose.
The stillness was broken when Renfrow stood up from his mat after three hours. He’d worn a sweatshirt to the ceremony with his initials, JR, emblazoned across the chest. He peeled the shirt off his body in frustration and tossed it aside.
Tears spilled down his face.
As the ceremony wound down, the athletes began sitting up, and a few chatted quietly.
Most weren’t sure how to describe the experience. For some, it felt like a descent into the recesses of the mind, with colors and emotions swirling together. Others said they confronted traumas they thought they’d buried, or emotions they wanted to suppress. They expressed feeling a connection to the other people in the circle.
“It’s the ultimate ego killer because, for me at least, it gives you incredible empathy that you’ve never felt before,” Lee said. “When you’re doing a journey with other people, you see yourself in them. It’s almost like you’re walking past a mirror, different mirrors. You see parts of yourself in everybody and you realize that we’re all connected and we’re all going through something, we’re all in some sort of pain, and it humbles you.”
Most of the athletes drifted off to be alone so they could scribble down their thoughts in a journal, per instructions from Wake staffers. There would be a communal therapy session the next morning.
Each would be asked to share something from their journey.
***
In the end, most of those curious about psilocybin simply want to know: Does it work? And how does it work? Scientists say those are difficult questions to answer right now.
Researchers have discovered that classic psychedelics, like psilocybin and LSD, act on the serotonin 2A receptor, the same receptor targeted by the most common antidepressants on the market. But beyond that, the understanding of how they work to help people is, at this point, more theory or conjecture than scientific fact.
Johnson, the Johns Hopkins researcher, said psilocybin helps increase openness in people, allowing them to step outside of their vision of who they are. Someone who is resigned to being a smoker who can’t quit or a person with depression who can’t find happiness can, under the influence of psychedelics, view themselves in a different way, he said.
“Once they’re outside of the mental trap, it just becomes so obvious to people with these different disorders that, ‘You know what? I can just decide to quit smoking. I can cast aside my sadness,’” Johnson said.
Studies with rats show that psychedelics also appear to increase neuronal connectivity in the brain, even after a single dose. That could help the brain recover from traumatic injuries or concussions, finding new pathways around damaged areas.
The prevailing theory of how psilocybin and other psychedelics might help treat mental health is that they tamp down activity in the brain’s default mode network. It’s a set of regions in the brain that are engaged when people are ruminating about something and one of the few parts that is overactive in people with depression.
They often revisit mistakes they’ve made over and over again or continually beat themselves up about them, said LaPratt, the Sheppard Pratt researcher. That overactivity in the default mode network leads to repetitive patterns of negative thoughts — What’s wrong with me? Why am I so unhappy? — from which the person cannot escape.
People with depression often ruminate about the past; people with anxiety, about the future.
“You may have something coming up and then the brain starts thinking, and again, like that broken record,” LaPratt said. “It can be very easy to start thinking about how everything might go wrong and start catastrophizing.”
That repetitive thinking prevails in people with other conditions, too, including obsessive compulsive disorder and post-traumatic stress disorder. It begins to affect their sense of who they are; they define themselves as their condition.
But psychedelics seem to help people examine old traumas without falling back into the same kind of destructive loop. They can help people feel more connected to others. Depression and anxiety aren’t simply erased, LaPratt said, but people can gain a new perspective on their problems and start to feel, maybe for the first time, that they can shake them off.
“We see increased openness and some motivation for changing behaviors,” he said.
Psychedelics are mostly out of a person’s system by the next morning, but, according to researchers, that increased openness can last for weeks or months without additional doses, providing a window during which they can begin to address their problems.
“It is maybe that we’re helping people get to the point of being able to accept the things they can’t change and to change the things that they can,” Aaronson said, echoing the Serenity Prayer, often used in 12-step recovery programs. “Personal autonomy is taken away from people with depression. They don’t feel like they can operate in their own best interest. They get caught in internal conflict. And I think this helps them get beyond that.”
***
In the morning, the athletes gathered on a patio for a form of group therapy called integration. It was scheduled to last at least two hours. Macleod explained it was an essential part of understanding a psilocybin journey. Every attendee had an opportunity to share something from their experience, whether it was enlightening, confusing, uplifting, or a mixture of many emotions.
Lee spoke about his anxiety, about trying to understand what his identity would be now that he wasn’t a boxer. By walking away from the ring, he feared he was letting down all the people who supported him when he chose a boxing career instead of a job in finance after he graduated from Notre Dame. But now he’d come to understand those were his own insecurities. He could walk his own path. He could help people experiencing similar physical and emotional pain.
Renfrow took several deep breaths as he searched for words. For most of his life, he’d viewed himself as a football player. But on his psilocybin journey, he felt as if members of his family told him it was OK to let go. When he stood up during the ceremony and peeled off his shirt with his initials, he said, he was symbolically letting go of something.
“It’s OK to stop chasing the football journey,” Renfrow said. “I’m not going to suit up this year and that’s cool with me. I’ll be able to figure it out.”
In saying goodbye to football, he said, he was saying goodbye to his grandmother.
“Football was her,” Renfrow said, and he began crying. “We went on all my recruiting trips. So I had to let her go with letting football go. And that was a big moment when I stood up. I had to let her go. So it was tough, but I had to do it.”
When it was Downie’s turn, he tried to defuse the tension by joking that it was time to go eat. He didn’t want to open up to the group, he said. He’d written some notes on a sheet of paper. His hands shook as he tried to read them.
“I wasn’t drinking and I wasn’t doing drugs for fun,” Downie said, his voice trembling. “I was numbing my brain because it was f—ed. I couldn’t turn out of my driveway for a year. I sat in dark rooms and I turned to drugs and alcohol.”
But on the psychedelic trip, he said, he was able to connect with his past. “I’m sitting there and I’m going through my brain, I’m talking to my dad, I’m talking to my family members. I’ve said sorry to everyone I could possibly say sorry to,” he said. “It made me cry. It made me feel good.”
He realized, through the journey, he wanted to be a better man. His voice was shaking as he tried to get the words out.
“At the end of all this, I think what I’ve learned is how to control what goes on. I do have control. I can control this,” he said. “I’m going to go home and I’m going to identify and execute and be a better father and stay around for my kids, deal with my concussion problems as best I can.”
He turned to look directly at Cote, tears streaming down his cheeks from behind his sunglasses.
“I mean this, bro, when I say you saved my life.”
As Downie’s words gave way to silence, Lee stood up from his chair. He crossed the circle, walked over to Downie, and opened his arms wide. The two fighters, who came to Jamaica sad and broken, embraced.
***
While studies have found that psilocybin plus therapy is more effective than therapy alone, it’s unclear whether psilocybin alone, without the preparatory work or the integration afterward, has any effect.
“There’s a reason why people who go to raves and take psilocybin don’t get cured,” Aaronson said. “Psilocybin is not an antidepressant.”
Even within strict clinical trial protocols, the question remains whether psilocybin-assisted therapy works. Preliminary studies have been promising, but the numbers of test subjects have been small. Much larger studies are needed to determine both safety and efficacy.
Still, that hasn’t stopped psilocybin advocates from touting the research to date, implying it is more definitive than it is. Moreover, many mushroom evangelists attribute the positive effects from clinical trials to taking psilocybin in general, discounting the protocols used in the studies.
The Wake retreat in Jamaica, for example, had the athletes take psilocybin in group ceremonies guided by Cowan, the local shaman, while the group integration sessions were led by an osteopathic physician. Neither was a licensed psychotherapist, Murray said. It’s unclear whether the benefits of psilocybin therapy suggested by clinical research would apply to a group setting — for the dosing or the integration.
Murray, Wake’s CEO, said that while clinical research strives to remove any variables, such as interactions between test subjects, Wake leaders feel the group setting offers benefits to its clients.
“It’s that group feeling that, ‘We’re in this together. My divorce is like your divorce. I lost a brother,’” he said. “That’s tough to put into a clinical trial.”
Wake had registered to hold a clinical trial in Jamaica, but Murray said the company ultimately decided not to pursue it, focusing on offering treatment instead.
Still, Murray said Wake is contributing to scientific research: They collected the blood and saliva samples, and participants were asked to fill out questionnaires before and after the retreat to help assess whether the treatment worked.
Murray said Wake uses the same clinically validated questionnaires used in a psychiatrist’s office. “So, it’s not theater. These are the actual tools that are used,” he said. It would be hard with Wake’s approach, however, to parse whether participants were helped by the mushrooms and integration or by other influences, such as being on vacation in Jamaica, being among a supportive peer group, or the marijuana many of them smoked regularly during the retreat.
“You’ve got to at least listen and take it seriously. There’s anecdotes of people saying they would have killed themselves,” Johnson said. “Sometimes you do see just the ‘full monty’ experience, where this person is just there on a dark, dark trajectory and their whole life changes. I suspect this is real. Something’s happening with these athletes making these reports.”
Glowing anecdotes, particularly when they come from high-profile athletes or celebrities, carry weight with the public and help spur measures like those in Oregon and Colorado that are establishing pathways to psilocybin treatment regardless of what researchers or regulators think.
“When people are upset and we’re not meeting their needs, they’re going to try things out,” said Atheir Abbas, an assistant professor of behavioral neuroscience at Oregon Health & Science University. “Hopefully, scientists can catch up to understanding why people think this is really helpful. And maybe it is helpful, but let’s try to figure out if it is and how.”
But there’s a danger in taking these stories, no matter how compelling, and extrapolating safety or efficacy from them.
“The hard part is the plural of anecdote is not data,” said Sabet, the Smart Approaches to Marijuana CEO. “And the data isn’t there yet.”
***
A year after the retreat, Downie, Renfrow, and Lee said they believed their psilocybin journey had helped them. It did not magically fix all their issues, but each considered it a positive experience.
Downie no longer feels that he is stuck in a dark place. When he returned to Ontario, he said, his family noticed a difference right away.
“That trip gave me a lot of clarity,” Downie said. “It gives you directions. It kind of gives you answers internally. It’s a unique thing I experienced. My year was definitely better than the previous year, that’s for sure. … Do I think it could help other people? I would say yes. Did it help me? Absolutely.”
No longer feeling like a prisoner in his house, Downie started a snowmobile camp that takes adults on guided adventures around Moosonee, near James Bay. It’s something he used to do with his family before his hockey career took off.
“It’s not much to brag about, but it’s the most northern you can go in Ontario in a snowmobile,” Downie said. “A lot of adults come from all over. It’s a pretty cool experience. It’s always been a passion of mine.”
He still has lingering issues from his concussions and suspects he always will.
“It is what it is,” he said. “Would I say it’s getting better? It’s a process.”
The most positive outcome has been the joy he’s found in being a father.
“My little guy is starting to fall in love with hockey, which is something I’ve been waiting for,” Downie said.
Although Downie hasn’t taken another psilocybin journey, he said he would be open to it.
Renfrow emerged from the ceremony intent on retiring from professional football but three months later re-signed with the Canadian Football League’s Edmonton Elks. This year, he joined the National Arena League’s Jacksonville Sharks, in part to be closer to his son.
“At that time, I thought I was going to quit football,” he said.
But he feels comfortable where he is and says he’s fulfilling his goals, including hosting that cooking show on YouTube he’d hoped to do. And he said he’s having fun again. He now turns to mushrooms whenever he has a big decision to make.
“I wholehearted believe in that and all the kind of guidance it’s given me,” he said. “You couldn’t ask for a better thing, to have followed guidance from a mushroom journey.”
Lee moved from California to Austin, Texas, and now runs a CBD business with his sister. Finding his post-boxing identity has remained a process. In his psychedelic journeys at the Wake retreat, Lee said, he was never thinking about sports or boxing. His visions were all about family, God, the universe.
“It kind of just makes me realize how much importance I’m putting on something that my subconscious doesn’t even care about,” he said. “My subconscious doesn’t care that I’m a boxer, that I was a fighter and did this and did that. It’s all kind of ego.”
The experience, he said, helped him understand how powerful the mind can be — that it can be a friend or a foe.
“I came away from it kind of realizing that I have all the tools to heal myself,” he said. “That’s huge. Because, especially for guys who have had concussions or athletes or what have you, you feel kind of isolated, you feel alone, you feel hopeless. So it kind of gives you a sense of hope.”
It allowed him to move beyond the need to prove himself, in the ring or outside it, to stop measuring his worth by his accomplishments. He’s become obsessed with much calmer, nonviolent pursuits: surfing and pickleball.
“I can turn my brain off just like in boxing,” he said. “But at the same time, it’s easier on my body and just, I don’t know, more fulfilling. I don’t have to prove anything.”
The Jamaican trip is allowing him to move forward, to do the work necessary to heal.
“Part of me went into it hoping that all my problems would be solved, but putting those expectations on it can be difficult,” he said. “Am I cured? No. But did it really help? And was it, like, one of the most profound experiences of my life?
“I’d say yes.”
This article was reported and written by KFF Health News’ Markian Hawryluk and ESPN’s Kevin Van Valkenburg. Researcher John Mastroberardino contributed to this report.
[Editor’s note: As part of the reporting of this article, some members of ESPN’s reporting team, under the guidance of Wake Network staff, used psilocybin. Wake Network was compensated, but not by ESPN.]
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
2 years 3 months ago
Health Industry, Mental Health, Pharmaceuticals, States, Colorado, Oregon, texas
Demand for home health aides is soaring. So why are they still so undervalued?
On most days around 2 p.m., home health aide Duane Crichlow can be found in an apartment in Sunset Park, Brooklyn, playing catch with his client — a man in his 30s with a developmental disability who is quick to give Crichlow hugs and kisses.
If it’s nice outside, Crichlow will walk his client, who is nonverbal and in a wheelchair half the time, down three flights of stairs, hauling the wheelchair back and forth separately.
A 49-year-old Trinidadian who lives in Bed-Stuy, Brooklyn, Crichlow works for St. Nicholas Alliance Home Care, where he earns between $17-$18 per hour. His client likes it when Crichlow imitates Mojo Jojo, a character from the TV series “The Powerpuff Girls,” or tries out Cardi B’s signature catchphrase, “Okurr.” “I do different characters that make him laugh. As long as he’s happy, I’m happy,” Crichlow said.
2 years 3 months ago
Health, Aging, caregiving, health care workers, Mental Health
News Archives - Healthy Caribbean Coalition
Caribbean Youth Mental Health Call to Action
Caribbean Youth Mental Health Call to Action
Block Title
@media only screen and (min-width:768px) and (max-width:1169px){}@media only screen and (max-width:767px){}
Sign the Call to Action
CountryAnguilla
Antigua and Barbuda
Aruba
The Bahamas
Barbados
Belize
Bermuda
Cayman Islands
Dominica
Dominican Republic
Grenada
Guadeloupe
Haiti
International
Jamaica
Martinique
Montserrat
Netherlands Antilles
Saint Kitts and Nevis
Saint Lucia
Saint Maarten
Saint Vincent and The Grenadines
Suriname
Trinidad and Tobago
Turks and Caicos Islands
Virgin Islands, British
Virgin Islands, U.S.
Sign Now
158
People support this cause
WHY SHOULD WE CARE ABOUT YOUTH MENTAL HEALTH?
Half of all mental health disorders can be diagnosed by just age 14.
16 million adolescents aged 10-19 live with a mental disorder in Latin America and the Caribbean.
Anxiety Disorder is the second leading cause of disability among 10-14-year-olds.
The post appeared first on Healthy Caribbean Coalition.
2 years 4 months ago
Healthy Caribbean Youth, Mental Health, News, Slider
Estrés pandémico, pandillas y miedo impulsaron un aumento de tiroteos adolescentes
Diego nunca imaginó que portaría un arma.
No lo pensó cuando niño, o durante un tiroteo fuera de su casa en el área de Chicago. Tampoco a los 12 años, cuando uno de sus amigos fue baleado.
Diego nunca imaginó que portaría un arma.
No lo pensó cuando niño, o durante un tiroteo fuera de su casa en el área de Chicago. Tampoco a los 12 años, cuando uno de sus amigos fue baleado.
La mente de Diego cambió a los 14, cuando él y sus amigos estaban listos para ir a la vigilia de Nuestra Señora de Guadalupe. Esa noche, en lugar de cánticos religiosos, escuchó disparos y gritos. Un pandillero le había disparado a dos personas, una de ellas un amigo suyo, quien recibió nueve balazos.
“Mi amigo se estaba desangrando”, dijo Diego, quien le pidió a KHN no utilizar su apellido para proteger su seguridad y privacidad. Mientras su amigo yacía en el suelo, “se estaba ahogando en su propia sangre”.
El ataque dejó al amigo de Diego paralizado de la cintura para abajo. Y a Diego, uno de un número creciente de adolescentes que son testigos de la violencia armada, traumatizado y con miedo de salir a la calle sin un arma.
Investigaciones muestran que los adolescentes expuestos a la violencia armada tienen el doble de probabilidades que otros de cometer un delito violento grave dentro de los dos años luego del trauma, lo que perpetúa un ciclo difícil de romper.
Diego pidió ayuda a sus amigos para tener una pistola y, en un país sobrecargado con armas de fuego, no tuvieron problemas para conseguirle una, que le dieron gratis.
“Me sentí más seguro con el arma”, dijo Diego, que ahora tiene 21 años. “Esperaba no usarla”.
Durante dos años, Diego mantuvo el arma solo como elemento de disuasión. Cuando finalmente apretó el gatillo, cambió su vida para siempre.
Tendencias inquietantes
Los medios de comunicación se centran en gran medida en los tiroteos masivos y el estado mental de las personas que los cometen.
Pero hay una epidemia mucho mayor de violencia armada —particularmente entre los jóvenes negros no hispanos, hispanos (que pueden ser de cualquier raza) y nativos americanos— que atrapa a muchos que ni siquiera tienen edad suficiente para obtener una licencia de conducir.
Estudios muestran que la exposición crónica al trauma puede cambiar la forma en que se desarrolla el cerebro de un niño. El trauma también puede desempeñar un papel central en la explicación de por qué algunos jóvenes buscan protección en las armas y terminan usándolas contra sus compañeros.
La cantidad de niños menores de 18 años que mataron a alguien con un arma de fuego aumentó de 836 en 2019 a 1,150 en 2020.
En la ciudad de Nueva York, la cantidad de jóvenes que mataron a alguien con un arma aumentó más del doble, pasando de 48 delincuentes juveniles en 2019 a 124 en 2022, según datos del departamento de policía de la ciudad.
La violencia armada juvenil aumentó más modestamente en otras ciudades; en muchos lugares, la cantidad de homicidios de adolescentes con armas de fuego subió en 2020, pero desde entonces se ha acercado a los niveles previos a la pandemia.
Investigadores que analizan las estadísticas del crimen enfatizan que los adolescentes no están impulsando el aumento general de la violencia armada, que ha aumentado en todas las edades. En 2020, el 7,5% de los arrestos por homicidio involucraron a menores de 18 años, una proporción ligeramente menor que en años anteriores.
A líderes locales les cuesta encontrar la mejor manera de responder a los tiroteos adolescentes.
Un puñado de comunidades, incluidas Pittsburgh; el condado de Fulton, en Georgia; y el condado de Prince George, en Maryland, han debatido o implementado toques de queda juveniles para frenar la violencia adolescente. Lo que no está en discusión: más personas de 1 a 19 años mueren por violencia armada que por cualquier otra causa.
Una vida de límites
El número devastador de la violencia armada se revela a diario en las salas de emergencia.
En el centro de trauma de UChicago Medicine, la cantidad de heridas de bala en menores de 16 años se ha duplicado en los últimos seis años, dijo el doctor Selwyn Rogers, director fundador del centro. La víctima más joven tenía 2 años.
“Escuchas a la madre gemir o al hermano decir: ‘No es cierto’”, dijo Rogers, quien trabaja con jóvenes locales como vicepresidente ejecutivo del hospital para salud comunitaria. “Tienes que estar presente en ese momento, pero luego salir por la puerta y lidiar con todo de nuevo”.
En los últimos años, el sistema judicial ha luchado por equilibrar la necesidad de seguridad pública con la compasión por los menores, según investigaciones que muestran que el cerebro de una persona joven no madura por completo hasta los 25 años.
La mayoría de los delincuentes jóvenes “superan la edad” del comportamiento delictivo o violento casi al mismo tiempo, a medida que desarrollan más autocontrol y habilidades de pensamiento de largo alcance.
Sin embargo, los adolescentes acusados de tiroteos a menudo son enjuiciados como adultos, lo que significa que enfrentan castigos más severos, dijo Josh Rovner, director de justicia juvenil en Sentencing Project, que aboga por la reforma del sistema judicial.
En 2019, aproximadamente 53,000 menores fueron acusados como adultos, lo que puede tener graves repercusiones para la salud. Estos adolescentes tienen más probabilidades de ser victimizados mientras están presos, dijo Rovner, y de ser arrestados nuevamente después de quedar libres.
Los jóvenes pueden pasar gran parte de sus vidas en un “aislamiento” impuesto por la pobreza, sin aventurarse más allá de sus vecindarios, aprendiendo poco sobre las oportunidades que existen en el resto del mundo, dijo Rogers. Millones de niños estadounidenses, en particular niños negros no hispanos, latinos y nativos americanos, viven en entornos plagados de pobreza, violencia y consumo de drogas.
La pandemia de covid-19 amplificó todos esos problemas, desde el desempleo hasta la inseguridad alimentaria y de vivienda.
Aunque nadie puede decir con certeza qué provocó el aumento de tiroteos en 2020, la investigación ha relacionado durante mucho tiempo la desesperanza y la falta de confianza en la policía, que aumentó después del asesinato de George Floyd ese año, con un mayor riesgo de violencia comunitaria.
Las ventas de armas se dispararon un 64% entre 2019 y 2020, mientras que se cancelaron muchos programas de prevención de la violencia.
Una de las pérdidas más graves que enfrentaron los niños durante la pandemia fue el cierre de las escuelas durante un año o más, justamente las instituciones que proporcionan tal vez la única fuerza estabilizadora en sus jóvenes vidas.
“La pandemia encendió el fuego debajo de la olla”, dijo Elise White, subdirectora de investigación Center for Justice Innovation, un entidad sin fines de lucro que trabaja con comunidades y sistemas de justicia. “Mirando hacia atrás, es fácil restar importancia ahora a lo incierto que se sintió ese momento [de la pandemia]. Cuanto más insegura se sienta la gente, cuanto más sientan que no hay seguridad a su alrededor, más probable es que porten armas”.
Por supuesto, la mayoría de los niños que experimentan dificultades nunca infringen la ley. Múltiples estudios han encontrado que la mayor parte de la violencia armada es perpetrada por un número relativamente pequeño de personas.
Incluso la presencia de un adulto solidario puede proteger a los niños de involucrarse en la delincuencia, explicó el doctor Abdullah Pratt, médico de emergencias de UChicago Medicine que perdió a su hermano por la violencia con armas de fuego.
Pratt también perdió a cuatro amigos por la violencia con armas durante la pandemia. Los cuatro murieron en su sala de emergencias; uno era el hijo de una enfermera del hospital.
Aunque Pratt creció en una parte de Chicago donde las pandillas callejeras eran comunes, se benefició del apoyo de padres amorosos y fuertes modelos a seguir, como maestros y entrenadores de fútbol americano. A Pratt también lo protegió su hermano mayor, quien lo cuidaba y se aseguraba de que las pandillas dejaran en paz al futuro médico.
“Todo lo que he podido lograr”, dijo Pratt, “es porque alguien me ayudó”.
Crecer en una “zona de guerra”
Diego no tenía adultos en casa que lo ayudaran a sentirse seguro.
A menudo, sus propios padres eran violentos. Una vez, en un ataque de ira por la borrachera, su padre lo agarró por la pierna y lo zarandeó por la habitación, contó Diego; y su madre una vez le arrojó una tostadora a su padre.
A los 12 años, los esfuerzos de Diego para ayudar a la familia a pagar las facturas atrasadas —vendiendo marihuana, y robando autos y apartamentos— llevaron a su padre a echarlo de la casa.
A los 13 años, Diego se unió a una pandilla del barrio. Los pandilleros, que contaron historias similares sobre huir del hogar para escapar del abuso, le dieron comida y un lugar para quedarse. “Éramos como una familia”, dijo Diego. Cuando tenían hambre y no había comida en casa, “íbamos juntos a una gasolinera a robar algo de desayuno”.
Pero Diego, que era más pequeño que la mayoría de los demás, vivía con miedo. A los 16, pesaba solo 100 libras. Los chicos más grandes lo intimidaban y lo golpeaban. Y su exitosa actividad, vender mercadería robada en la calle por dinero en efectivo, llamó la atención de pandilleros rivales, quienes amenazaron con robarle.
Los niños que experimentan violencia crónica pueden desarrollar una “mentalidad de zona de guerra”, volviéndose hipervigilantes ante las amenazas, a veces sintiendo peligro donde no existe, dijo James Garbarino, profesor emérito de psicología en la Universidad de Cornell y la Universidad de Loyola-Chicago.
Los niños que viven con miedo constante tienen más probabilidades de buscar protección en las armas de fuego o en las pandillas. Se puede activar para que tomen medidas preventivas, como disparar un arma sin pensar, contra lo que perciben como una amenaza.
“Sus cuerpos están constantemente listos para pelear”, dijo Gianna Tran, subdirectora ejecutiva del East Bay Asian Youth Center en Oakland, California, que trabaja con jóvenes en riesgo.
A diferencia de los perpetradores de tiroteos masivos, que compran armas y municiones porque tienen la intención de asesinar, la mayor parte de la violencia adolescente no es premeditada, dijo Garbarino.
En las encuestas, la mayoría de los jóvenes que portan armas, incluidos los pandilleros, dicen que lo hacen por miedo o para disuadir ataques, en lugar de perpetrarlos. Pero el miedo a la violencia comunitaria, tanto de los rivales como de la policía, puede avivar una carrera armamentista urbana, en la que los menores sienten que solo los tontos no portan armas.
“Fundamentalmente, la violencia es una enfermedad contagiosa”, dijo el doctor Gary Slutkin, fundador de Cure Violence Global, que trabaja para prevenir la violencia comunitaria.
Aunque un pequeño número de adolescentes se vuelven duros y despiadados, Pratt dijo que ve muchos más tiroteos causados por la “pobre resolución de un conflicto” y la impulsividad de los adolescentes en lugar de un deseo de matar.
De hecho, las armas de fuego y un cerebro adolescente inmaduro son una mezcla peligrosa, enfatizó Garbarino. El alcohol y las drogas pueden aumentar el riesgo. Cuando se enfrentan a una situación potencialmente de vida o muerte, pueden actuar sin pensar.
Cuando Diego tenía 16 años, estaba acompañando a una niña a la escuela y se les acercaron tres jóvenes, incluido un pandillero, quien, usando un lenguaje obsceno y amenazante, le preguntó a Diego si también estaba en una pandilla. Diego dijo que trató de pasar de largo, y uno de ellos parecía tener un arma.
“No sabía cómo disparar un arma”, dijo Diego. “Solo quería que huyeran”.
En las noticias sobre el tiroteo, testigos dijeron que escucharon cinco disparos. “Lo único que recuerdo es el sonido de los disparos”, dijo Diego. “Todo lo demás fue en cámara lenta”.
Diego había disparado a dos de los muchachos en las piernas. La niña corrió por un lado y él por otro. La policía lo arrestó en su casa unas horas después. Fue juzgado como adulto, condenado por dos cargos de intento de homicidio y sentenciado a 12 años.
Una segunda oportunidad
En las últimas dos décadas, el sistema judicial ha realizado cambios importantes en la forma en que trata a los niños.
Los arrestos de jóvenes por delitos violentos bajaron dramáticamente un 67% entre 2006 y 2020, y 40 estados han hecho que sea más difícil acusar a menores como adultos.
Los estados también están adoptando alternativas a la cárcel, como hogares grupales que permiten a los adolescentes permanecer en sus comunidades, al tiempo que brindan tratamiento para ayudarlos a cambiar su conducta.
Debido a que Diego tenía 17 años cuando fue sentenciado, fue enviado a un centro de menores, donde recibió terapia por primera vez.
Diego terminó la escuela secundaria mientras estaba tras las rejas, y obtuvo un título de un colegio comunitario. Con otros jóvenes reclusos fue de excursión a teatros y al acuario, lugares en los que nunca había estado. La directora del centro de detención le pidió que la acompañara a eventos sobre la reforma de la justicia juvenil, donde lo invitaron a contar su historia.
Para Diego, esas fueron experiencias reveladoras: se dio cuenta de que había visto muy poco de Chicago, a pesar de que había pasado su vida allí.
“Mientras estás creciendo, lo único que ves es a tu comunidad”, dijo Diego, quien fue liberado después de cuatro años, cuando el gobernador conmutó su sentencia. “Asumes que el mundo entero es así”.
La editora de datos de KHN Holly K. Hacker y la investigadora Megan Kalata contribuyeron con este informe.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
USE OUR CONTENT
This story can be republished for free (details).
2 years 4 months ago
Mental Health, Noticias En Español, Race and Health, Children's Health, Guns, Illinois
Seniors With Anxiety Frequently Don’t Get Help. Here’s Why.
Anxiety is the most common psychological disorder affecting adults in the U.S. In older people, it’s associated with considerable distress as well as ill health, diminished quality of life, and elevated rates of disability.
Yet, when the U.S. Preventive Services Task Force, an independent, influential panel of experts, suggested last year that adults be screened for anxiety, it left out one group — people 65 and older.
The major reason the task force cited in draft recommendations issued in September: “the current evidence is insufficient to assess the balance of benefits and harms of screening for anxiety” in all older adults. (Final recommendations are expected later this year.)
The task force noted that questionnaires used to screen for anxiety may be unreliable for older adults. Screening entails evaluating people who don’t have obvious symptoms of worrisome medical or psychological conditions.
“We recognize that many older adults experience mental health conditions like anxiety” and “we are calling urgently for more research,” said Lori Pbert, associate chief of the preventive and behavioral medicine division at the University of Massachusetts Chan Medical School and a former task force member who worked on the anxiety recommendations.
This “we don’t know enough yet” stance doesn’t sit well with some experts who study and treat seniors with anxiety. Dr. Carmen Andreescu, an associate professor of psychiatry at the University of Pittsburgh, called the task force’s position “baffling” because “it’s well established that anxiety isn’t uncommon in older adults and effective treatments exist.”
“I cannot think of any danger in identifying anxiety in older adults, especially because doing so has no harm and we can do things to reduce it,” said Dr. Helen Lavretsky, a psychology professor at UCLA.
In a recent editorial in JAMA Psychiatry, Andreescu and Lavretsky noted that only about one-third of seniors with generalized anxiety disorder — intense, persistent worry about everyday matters — receive treatment. That’s concerning, they said, considering evidence of links between anxiety and stroke, heart failure, coronary artery disease, autoimmune illness, and neurodegenerative disorders such as dementia.
Other forms of anxiety commonly undetected and untreated in seniors include phobias (like a fear of dogs), obsessive-compulsive disorder, panic disorder, social anxiety disorder (a fear of being assessed and judged by others), and post-traumatic stress disorder.
The smoldering disagreement over screening calls attention to the significance of anxiety in later life — a concern heightened during the covid-19 pandemic, which magnified stress and worry among seniors. Here’s what you should know.
Anxiety is common. According to a book chapter published in 2020, authored by Andreescu and a colleague, up to 15% of people 65 and older who live outside nursing homes or other facilities have a diagnosable anxiety condition.
As many as half have symptoms of anxiety — irritability, worry, restlessness, decreased concentration, sleep changes, fatigue, avoidant behaviors — that can be distressing but don’t justify a diagnosis, the study noted.
Most seniors with anxiety have struggled with this condition since earlier in life, but the way it manifests may change over time. Specifically, older adults tend to be more anxious about issues such as illness, the loss of family and friends, retirement, and cognitive declines, experts said. Only a small fraction develop anxiety after turning 65.
Anxiety can be difficult to identify in older adults. Older adults often minimize symptoms of anxiety, thinking “this is what getting older is like” rather than “this is a problem that I should do something about,” Andreescu said.
Also, seniors are more likely than younger adults to report “somatic” complaints — physical symptoms such as dizziness, fatigue, headaches, chest pain, shortness of breath, and gastrointestinal problems — that can be difficult to distinguish from underlying medical conditions, according to Gretchen Brenes, a professor of gerontology and geriatric medicine at Wake Forest University School of Medicine.
Some types of anxiety or anxious behaviors — notably, hoarding and fear of falling — are much more common in older adults, but questionnaires meant to identify anxiety don’t typically ask about those issues, said Dr. Jordan Karp, chair of psychiatry at the University of Arizona College of Medicine in Tucson.
When older adults voice concerns, medical providers too often dismiss them as normal, given the challenges of aging, said Dr. Eric Lenze, head of psychiatry at Washington University School of Medicine in St. Louis and the third author of the recent JAMA Psychiatry editorial.
Simple questions can help identify whether an older adult needs to be evaluated for anxiety, he and other experts suggested: Do you have recurrent worries that are hard to control? Are you having trouble sleeping? Have you been feeling more irritable, stressed, or nervous? Are you having trouble with concentration or thinking? Are you avoiding things you normally like to do because you’re wrapped up in your worries?
Stephen Snyder, 67, who lives in Zelienople, Pennsylvania, and was diagnosed with generalized anxiety disorder in March 2019, would answer “yes” to many of these queries. “I’m a Type A personality and I worry a lot about a lot of things — my family, my finances, the future,” he told me. “Also, I’ve tended to dwell on things that happened in the past and get all worked up.”
Treatments are effective. Psychotherapy — particularly cognitive behavioral therapy, which helps people address persistent negative thoughts — is generally considered the first line of anxiety treatment in older adults. In an evidence review for the task force, researchers noted that this type of therapy helps reduce anxiety in seniors seen in primary care settings.
Also recommended, Lenze noted, is relaxation therapy, which can involve deep breathing exercises, massage or music therapy, yoga, and progressive muscle relaxation.
Because mental health practitioners, especially those who specialize in seniors’ mental health, are extremely difficult to find, primary care physicians often recommend medications to ease anxiety. Two categories of drugs — antidepressants known as SSRIs (selective serotonin reuptake inhibitors) and SNRIs (serotonin-norepinephrine reuptake inhibitors) — are typically prescribed, and both appear to help to older adults, experts said.
Frequently prescribed to older adults, but to be avoided by them, are benzodiazepines, a class of sedating medications such as Valium, Ativan, Xanax, and Klonopin. The American Geriatrics Society has warned medical providers not to use these in older adults, except when other therapies have failed, because they are addictive and significantly increase the risk of hip fractures, falls and other accidents, and short-term cognitive impairments.
We’re eager to hear from readers about questions you’d like answered, problems you’ve been having with your care, and advice you need in dealing with the health care system. Visit khn.org/columnists to submit your requests or tips.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
USE OUR CONTENT
This story can be republished for free (details).
2 years 4 months ago
Aging, Health Industry, Mental Health, Navigating Aging, Pennsylvania